Efforts to reduce the excess risk of dying from cancer faced by people living in countries of Eastern and Central Europe, compared with their Western counterparts have been high on the European agenda for the best part of two decades.
In 2005 a group of European Parliamentarians launched MEPs Against Cancer, to promote policy initiatives at EU and member state level. In 2009 the first of a succession of European Joint Actions – the European Partnership for Action Against Cancer – was launched. These Joint Actions offered a forum for very fruitful collaboration between cancer organisations and health ministries, and is widely recognised to have delivered some very valuable conceptual and practical tools, including guidelines for developing quality National Cancer Control Programmes, and principles for organising Comprehensive Cancer Care Networks. That body of work helped pave the way for the EU’s Europe’s Beating Cancer plan – a comprehensive policy document, launched by the European Commission in 2022, which has tackling disparities in access and outcomes at its heart.
Despite these sustained collaborative efforts, however, recent studies call into question the progress made so far in closing the East-West gap in cancer mortality rates. A 2022 Italian study, published in the European Journal of Cancer, which looked at the period from 1990 to 2016 found that, although mortality rates have fallen across Europe, “the gap between western and eastern areas persists in absolute terms and – if anything – became larger in relative terms.” While cancer mortality declined by 1–1.4% annually in Western Europe between 1990 and 2016, saving an estimated 3.9 million lives, “no material progress” was observed in Eastern Europe over that period. They estimated that, over that 25-year period, the relative excess mortality in Eastern countries grew from 32% to 37% in men, and from 15% to 21% in women.
A 2024 study, led by Maria Asensio, a principal researcher at Instituto Nacional de Administração, Portugal, which looked at data for 2020, painted a similar picture, though that study was confined to EU member states (plus Switzerland). They found that, compared with Nordic and Southern EU countries, age-standardised mortality rates are 35% higher in Central Eastern and South Eastern EU countries and around 25% higher the Baltic states.
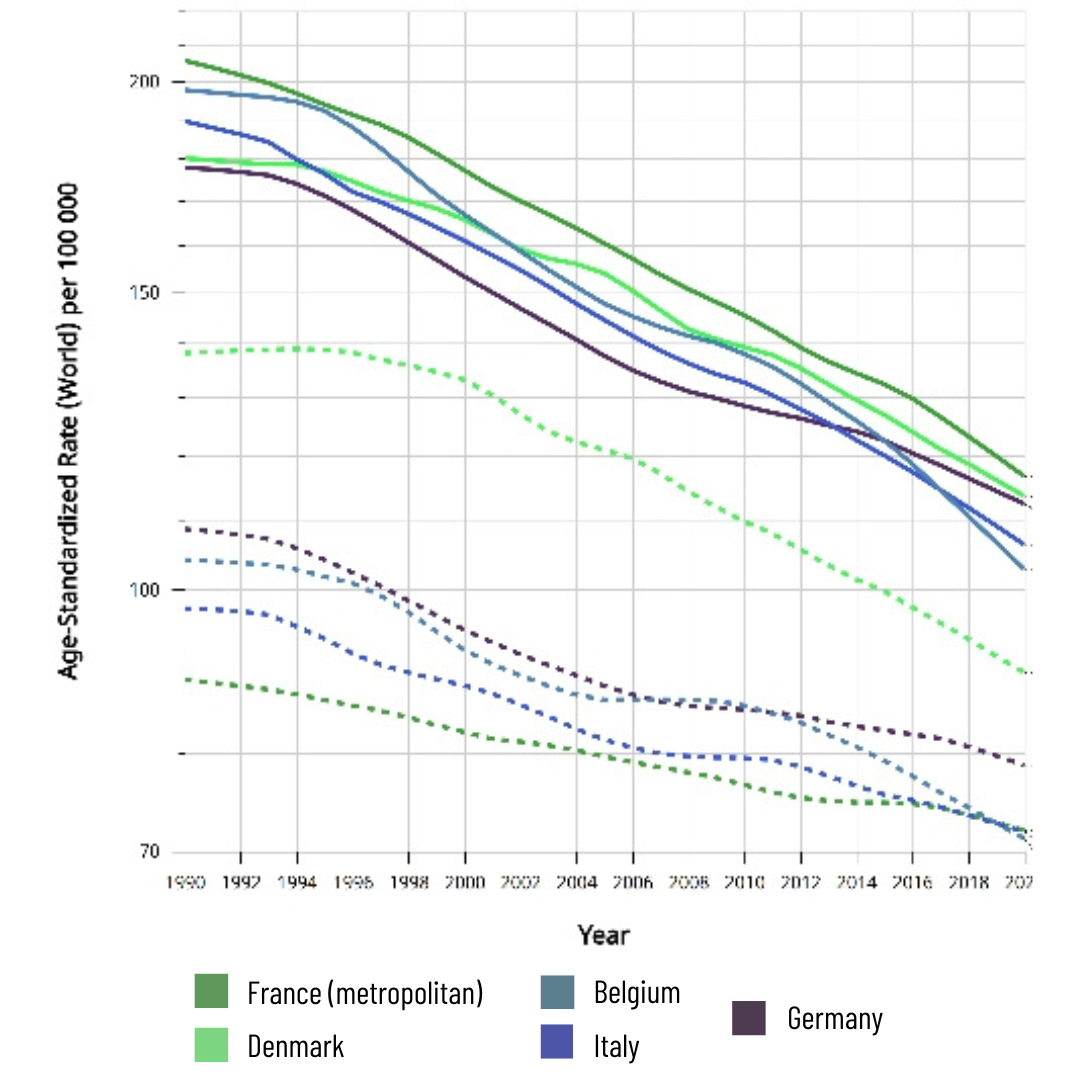
Western Europe (selected EU member states)
Eastern Europe (selected EU member states)
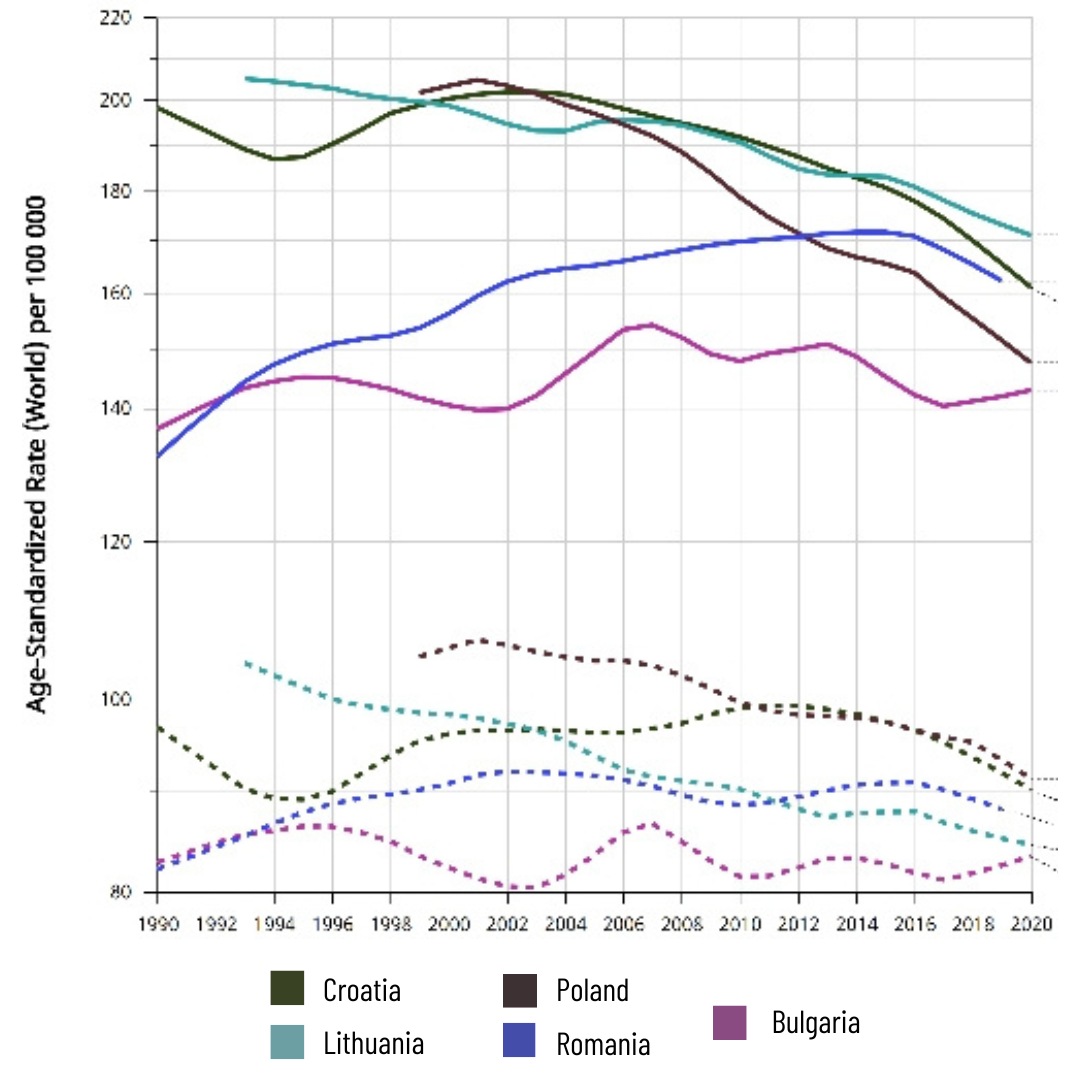
Source: Cancer Over time | IARC – https://gco.iarc.who.int © All Rights Reserved 2024
So what’s going wrong?
The Italian study, led by Claudia Santucci from the Università degli Studi di Milano Statale, made a detailed analysis of the excess mortality rate by cancer types, and explored the likely reasons in each instance. The problems were spread across the entire cancer control continuum – “differences in lifestyle patterns, mainly smoking and alcohol, besides different roll-out of improvements in cancer diagnosis and management are the key determinants of the persisting difference in cancer mortality between western and eastern Europe.”
That analysis would indicate that the strategy of developing quality national cancer control programmes that address every aspect of cancer control, from prevention, early detection and screening to the quality of diagnostics, treatment and care and effective organisation and governance of cancer services, is the right way to go. Developing such programmes, plans or strategies has been a recommendation from the EU since 2009. A survey conducted in 2016 showed that 28 countries did have such a plan, and in many cases the plan had been updated at least once since its launch.
The same survey showed, however, that only 11 of the 28 plans included all the elements listed in the quality guide. More importantly, perhaps, only 15 were backed by specific funding commitments, and that the lack of dedicated funding threatened the chances of successful implementation. The authors of the survey report noted that, “Despite evidence of a historically large and growing cancer burden, cancer services have not generally been prioritised in low- and lower-middle income countries by national governments or external funders.” They highlighted as the main deficient areas in national cancer control programmes, “the economics of cancer care and control as well planning of resources for cancer care.”
“Cancer services have not generally been prioritised in low- and lower-middle income countries by national governments or external funders”
Their conclusions chime closely with the analysis presented in the 2024 study led by Asensio, into the factors underlying their finding of a 35% excess mortality rate in Central Eastern and South Eastern EU countries, and a 25% excess mortality rate in Baltic countries, compared with Nordic and Southern EU countries. That study looked at how various characteristics of healthcare systems correlate with cancer mortality rates.
Regression analyses highlighted as key factors: health expenditure as a proportion of GDP; the degree of universal health coverage (i.e. healthcare services available with no financial barrier); and the availability of public cancer centres. All of those metrics were more favourable in high-income than low-income countries.
Specifically, they found “a pattern within Baltic European countries (i.e., Latvia, Estonia, and Lithuania), Southeastern European countries (i.e., Bulgaria, Croatia, and Romania), and Central Eastern European countries (i.e., Czechia, Hungary, Poland, Slovakia, and Slovenia), indicating higher age-standardised mortality rates in 2020, alongside lower health expenditure as a percentage of GDP and reduced UHC [universal health coverage] services.”
The study also highlighted correlations indicating that improving early detection rates is essential for success in cutting mortality rates, recommending that a threshold of 60% of invasive cancers detected at stage I or II seems to be significant for effective cancer downstaging efforts.
A question of priorities
The bottom line then would seem to be that Eastern European countries, several of which are still grappling with the economic consequences of post-Soviet transition, tend to allocate less to healthcare than their wealthier Western neighbours. Limited healthcare investment leads to poorer cancer outcomes, with prevention, early detection and poorer quality treatment all factors that play a greater or lesser role, depending on the cancer type.
When cancers go undiagnosed until they are advanced, treatment becomes more complex, less effective and more expensive.
Rural–urban divides in access to healthcare services, including screening, diagnostic facilities and specialist treatment, may also contribute to the persistent East-West gap in cancer mortality rates, as Eastern European countries tend to have a larger proportion of their populations living in rural areas. A 2014 survey, for instance, found that, in Romania, Croatia and Bulgaria, unmet needs for healthcare were at least 3.0 percentage points higher among rural dwellers compared to those living in cities or towns.
The concept of developing comprehensive cancer care networks in such a way as to provide entry points for high-quality diagnostics and care as close as possible to where people live – an approach currently being piloted in Czechia – could be an effective way to address this problem.
As with implementing measures outlined in national comprehensive cancer programmes, however, that will require governments in Eastern Europe to invest. Going by the evidence of the past two decades, it would seem that the key factor behind closing the gap in cancer mortality rates across Europe comes down to winning the argument, within the countries of Eastern Europe, in favour of giving a higher priority to spending on health and cancer care.
With that in mind, it is worth noting that, while Cancerworld has been able to draw on well-researched Europe-level studies for this article, trying to find experts and sources to speak to their own national situations proved challenging. Change will only come through transparency and open discussion. The alternative serves only to mask the problems and reinforce the barriers that prevent progress in improving cancer prevention and treatment across the region.
The opening map infographic is based on data for 2020, taken from the International Agency for Research on Cancer’s GLOBOCAN database, as presented in Asensio, M., & Amaral, E. (2024). Disparities in cancer outcomes: A comprehensive analysis of cancer incidence, mortality, and prevalence in Europe. Global Health Econ Sustain 2:3216.