When I got sick, I warned my friends: Don’t try to make me stop thinking about death.
Before I got sick, I’d been making plans for a place for public weeping, hoping to install in major cities a temple where anyone who needed it could get together to cry in good company and with the proper equipment. It would be a precisely imagined architecture of sadness: gargoyles made of night sweat, moldings made of longest minutes, support beams made of I-can’t-go-on-I-must-go-on.
When planning the temple, I remembered the existence of people who hate those they call crybabies, and how they might respond with rage to a place full of distraught strangers—a place that exposed suffering as what is shared. It would have been something tremendous to offer those sufferers the exquisite comforts of stately marble troughs in which to collectivize their tears. But I never did this.
Later, when I was sick, I was on a chemotherapy drug with a side effect of endless crying, tears dripping without agency from my eyes no matter what I was feeling or where I was. For months, my body’s sadness disregarded my mind’s attempts to convince me that I was O.K. I cried every minute, whether I was sad or not, my self a mobile, embarrassed monument of tears. I didn’t need to build the temple for weeping, then, having been one. I’ve just always hated it when anyone suffers alone.
The surgeon says the greatest risk factor for breast cancer is having breasts. She won’t give me the initial results of the biopsy if I am alone. My friend Cara, who works for an hourly wage and has no time off, drives out to the suburban medical office on her lunch break so that I can get my diagnosis. In the United States, if you aren’t someone’s child or parent or spouse, the law does not guarantee you leave from work to take care of them.
As Cara and I sit in the skylighted beige of the conference room, waiting for the surgeon to arrive, Cara gives me the small knife she carries in her purse so that I can hold on to it under the table. After all these theatrical prerequisites, what the surgeon says is what we already know: I have at least one cancerous tumor, 3.8 centimetres in diameter, in my left breast. I hand the knife back to Cara damp with sweat. She then returns to work.
No one knows you have cancer until you tell them. I take a screen capture of John Donne’s first devotion—the one that wonders what use it is to be an earth when earths are subject to earthquakes—and post it to Facebook: “We study health, and we deliberate upon our meats, and drink, and air, and exercises, and we hew, and we polish every stone that goes to that building; and so our health is a long and a regular work; but in a minute a cannon batters all.” It gets a lot of likes. Then I follow the other instructions I find on the Internet: tell my mother, tell my teen-age daughter, deep-clean the kitchen, negotiate with my employer, find someone to watch the cat, go to the thrift store to find clothes that will accommodate my coming chemo port, worry on the phone to my friends that I—a single working mother—have no one to take care of me. Because it is decided without ceremony that the doctors will eventually take my breasts from me and discard them in an incinerator, I begin the practice of pretending that my breasts were never there.
The cancer pavilion is a cruel democracy of appearance: the same bald heads, the same devastated complexions, the same steroid-swollen faces, the same plastic ports visible as lumps under the skin. The old seem infantile, the young act senile, the middle-aged find that all that is middle-aged about them disappears. The boundaries of our bodies break. Everything we were supposed to keep inside us now seems to fall out. Blood from chemotherapy-induced nosebleeds drips on the sheets, the paperwork, the CVS receipts, the library books. We emit foul odors. We throw up. We have poisonous vaginas and poisoned sperm. Because our urine is full of toxins, the signs in the bathroom instruct patients to flush twice.
Ten days after my diagnosis, doxorubicin will be infused into my body through a port surgically implanted in my chest and connected to my jugular vein. Its name is derived from “ruby,” because it is a brilliant and voluptuous red. One brand of the drug, Adriamycin, is named for the Adriatic Sea, near where it was discovered. I like to think of this poison as the ruby of the Adriatic, where I have never been but would like to go, but it is also called “the red devil,” and sometimes it is called “the red death.”
When administering the medicine, the oncology nurse must dress in an elaborate protective costume and slowly push the doxorubicin through the port. The medicine is so powerful that if it were to leak into the body it could cause my tissues to die. For several days after the drug is administered, my body’s fluids will be toxic to other people. Doxorubicin is sometimes fatal to the heart; a person can tolerate only a certain amount in a lifetime, and by the end of this treatment I will have reached half my limit.
Scientists discovered the drug known as the red devil near Castel del Monte, built by the Holy Roman Emperor Frederick II, in Italy, in the mid-thirteenth century. The castle had neither a moat nor a drawbridge, so few people believe that it was ever used as a fortress. It was built in a rare octagonal shape, and later it became a prison, then a refuge during the plague. In the seventeen-fifties, the Bourbons stripped out its marble. Two centuries later, scientists harvested its dirt. They took the castle soil to Milan, and found Streptomyces peucetius, the bright-red bacteria from which my treatment comes. Among its other effects, doxorubicin inhibits the enzyme topoisomerase II, slowing the rapid proliferation of cells. Many of these cells we need, but ideally many of them we don’t.
In the United States, doxorubicin was widely approved for use in 1974, the year after I was born. It is probably the same treatment that Susan Sontag was given before she wrote “Illness as Metaphor,” one of the first books someone mails to me when I fall ill. Treatment with doxorubicin can cause infection, leukemia, heart failure, and organ failure, and will almost certainly, for me, cause infertility. Because doxorubicin is a generalist in its destruction, it is also harmful to the central nervous system. The damage it unleashes cascades beyond treatment, and is often sustained for years. As I sit in the infusion chair, a drug cocktail pouring into me, the white and gray matter of my brain is under attack. There is no particular way to know how this will change me.
Doctors at first did not believe patients who described doxorubicin’s cognitive effects, or minimized the patients’ complaints as cancer-related unhappiness. MRIs of people who have had this chemotherapy for breast cancer indicate damage to the premotor and prefrontal cortices. Patients report that they lose the ability to read, to recall words, to speak fluently, to make decisions, and to remember. Some lose not just their short-term memories but their episodic ones—the memories of their lives.
I was given doxorubicin with cyclophosphamide, a drug approved for use in 1959, in a common treatment combination called dose-dense A.C. chemo. Cyclophosphamide is a medicalized form of a chemical weapon developed by Bayer scientists under the name lost and outlawed in 1925. Mustard gas, as it is also known, has always done its worst as an incapacitant rather than as a killer, but it can kill a person, too. During the war, lost filled the trenches with brilliant-yellow plumes. During cancer, it comes in plastic pouches, and no one in the pavilion speaks frankly about what it is.
Although four dose-dense rounds effectively eliminated many parts of me, neither of these drugs appeared to significantly reduce my tumor. After we were done with all that cellular annihilation, my own semi-annihilation was obvious, but my tumor remained intact. It remained as the full measure of shadow against the radiance of the screen.
Once my hair is gone, once I can no longer taste my food, once I have passed out while shopping for a bread knife in ikea, once the ex-lovers have all visited to make one last attempt to get me in bed, once the generous humiliations of crowdsourced charity have assured me months of organic produce, I have become a patient. The old ways are through. Any horizon is made of medicine. Any markers of specific identity beyond “the sick” and “the healthy” come from another era.
Every movie I watch now is a movie about an entire cast of people who seem not to have cancer, or, at least, this seems to me to be the plot. Any crowd not in the clinic is a crowd that feels curated by alienation, all the people everywhere looking robust and eyelashed and as if they have appetites for dinner and solid plans for retirement. I am marked by cancer, and I can’t quite remember what the markers are that mark us as who we are when we are not being marked by something else.
Yet I know I existed before I was ill. I kept journals, so I have proof. On the first day of 2014, the year in which I will fall ill, I am forty years old, teach art students for a living, and have a daughter in the eighth grade. We live in a two-bedroom apartment in suburban Kansas City, for which I pay around eight hundred and fifty dollars a month. According to my journals, where I dutifully record each day’s mundane details, I am wearing an oversized moth-eaten red cashmere sweater that I bought from the Salvation Army, and I seem to have a slight cold. I write that I am optimistic about starting out the New Year with a virus. It is as if the old year is being burned out of me through fever and the new one will come in renewed, because any illness that doesn’t kill you sets you on fire and then you start over, just like that. I am awaiting the next day’s delivery of a vintage Queen Anne-style fourposter bed, which I bought for two hundred and eighty dollars at a consignment shop. Twenty-six weeks into owning it, the week after my forty-first birthday, it becomes my sickbed.
Harriet Martineau, in her 1844 book, “Life in the Sick-Room,” wrote, “Nothing is more impossible to represent in words . . . than what it is to lie on the verge of life and watch, with nothing to do but to think, and learn from what we behold.” Virginia Woolf’s mother, Julia Stephen, also wrote a treatise on sickrooms. In this 1883 work, she instructed caregivers that, while the patient in a sickbed may have “fancies” that “seem, and often are, absurd,” these are heightened perceptions of the real, a result of the “delicately organised” minds of the very ill, “whose senses have become so acute through suffering.”
All that time lying down can also bring about the microscopic practice of worry. In the sickbed, illness illuminates shabbiness, self-absorption, inconsequence. I worry about personal finance, home economics, the social order. Virginia Woolf’s mother understood these agonists to the ill: “Among the number of small evils which haunt illness, the greatest, in the misery which it can cause, though the smallest in size, is crumbs. The origin of most things has been decided on, but the origin of crumbs in bed has never excited sufficient attention among the scientific world.”
Being sick makes excessive space for thinking, and excessive thinking makes room for thoughts of death. But I was always starving for experience, not its cessation, and, if the experience of thought was the only experience my body could give me beyond the one of pain, then opening myself to wild, deathly thinking had to be allowed. I warned my friends in a set of e-mailed instructions: Don’t try to make me stop thinking about death.
In the week before chemotherapy begins, it is like preparing for a winter storm, or a winter storm and a house guest, or a winter storm, a house guest, and the birth of a child. The day before chemotherapy, a friend arrives from someplace I would rather be—California or Vermont or two different towns named Athens. I do everything to look healthy so that my friend will praise the skillfulness of my camouflage, its materials purchased at Wigs.com, CVS, and Sephora. We don’t speak of chemotherapy except for the practical exchange of information, like what time to set the alarm for and the best route to the pavilion. We pass our time as friends would, roasting vegetables and listening to music and speaking excitedly of other friends or ideas or political events. The day of chemotherapy, we wake up early and arrive at least fifteen minutes late. We predict how well the treatment will go by what song is playing on the car radio: “Bohemian Rhapsody” (not so good), TLC’s “Waterfalls” (better). Chemotherapy, like most medical treatments, is boring. Like death, it is a lot of waiting for your name to be called. It is also waiting while the potential for panic and pain hangs around, too.
A nurse inserts a large needle into my subdermal port. First, things are drawn from me, then things are flushed in and out of me, then things drip into me. For each of these things that drip into me, I must say my name and when I was born. Of the many drugs that I am infused with, some have familiar, clear-cut effects: Benadryl, steroids, Ativan. I should know how these feel, but in this context they never feel like themselves. Instead, they combine with the chemotherapy drugs to create a new feeling, a unique mush of lack of clarity.
I was once a prompt person. Now I am always late. I was once a person who responded strongly to a cup of coffee. Now I am a person who behaves semi-unreactively with the sludge of substances inside me. I explain to my friend, as I am being infused, “They are giving me all the drugs, every last one of them.” The oncology nurse agrees: “Yes, we are. We are giving her all the drugs.”
I try to be the best-dressed person in the infusion room. I wrap myself up in thrift-store luxury and pin it together with a large gold brooch in the shape of a horseshoe. The nurses always praise the way I dress. I need that. Then they infuse me with a platinum agent, among other things, and I am a person in thrift-store luxury with platinum running through her veins.
A little kid sits on a couch with a large sign announcing his next tantrum.
After the infusion is done, I sit up until I fall over. I don’t give up until I give up. I try to win all the board games, remember all the books any of us have read, stay up late. Terrible things are happening in my body. Sometimes I will say it to my companions: “Terrible things are happening inside of me.” Finally, forty or forty-eight or sixty hours later, I can’t move and there is nothing to take for the pain, but, trying to be obedient to medicine and polite to my friends, I take something for the pain.
People with breast cancer are supposed to be ourselves as we were before, but also better and stronger and at the same time heart-wrenchingly worse. We are supposed to keep our unhappiness to ourselves but donate our courage to everyone. We are supposed to, as anyone can see in the YouTube videos, dance toward our mastectomies, or, as in “Sex and the City,” stand up with Samantha in the ballroom and throw off our wigs while a crowd of banqueting women and men roars with approval. We are supposed to, as Dana does in “The L Word,” pick ourselves up out of dreary self-pity and look stylish on the streets in our colorful hats. If we die later, as Dana does, we are supposed to know that our friends will participate in a fund-raising athletic event and take a minute, before moving on to other episodes, to remember that we once lived.
We are supposed to be legible as patients while navigating hospitals and getting treatment, and illegible as our actual, sick selves while going to work and taking care of others. Our actual selves must now wear the false heroics of disease: every patient a celebrity survivor, smiling before the surgery and smiling after it, too. We are supposed to be feisty, sexy, snarky women, or girls, or ladies, or whatever. Also, as the T-shirts for sale on Amazon suggest, we are always supposed to be able to tell cancer that “you messed with the wrong bitch!” In my case, however, cancer messed with the right bitch.
During treatment, you must have a desire to live, but it is also necessary to believe that you are a person worth keeping alive. Cancer requires painful, expensive, environmentally harmful, extractive medicine. My desire to survive means that I still can’t bring myself to unravel survival’s ethics. Many of the chemotherapy drugs I take, like cyclophosphamide, pass from urine into wastewater, and traces of them may last in the common water supply for up to eight hundred days. Another, carboplatin, accumulates in aquatic environments, where it lingers, but no one yet knows what damage it does. The West Himalayan yew tree, from which one of my drugs is harvested, has been endangered since 2011.
In 2017, a hundred and thirty billion dollars was spent on cancer drugs globally, an amount greater than the G.D.P. of more than a hundred countries. The cost of one chemotherapy infusion was more money than I had earned in any year of my life. My problem is that I want to live millions of dollars’ worth of life but cannot say why I deserve the extravagance of this existence. How many books, to pay back the world for my still existing, would I have to write?
While I was recovering from one of my treatments, I asked a friend to help me count my wounds. She said, “I don’t like this,” and looked like she was about to cry, like this was the sort of event that would end up in literature later, and I pleaded with her. I said, “This is my body,” and “I want to know what has happened to it.” I stood in front of a mirror with my compression garment pulled down past my waist. We looked at what we could see, she with horror, I with harsh, curious insistence. We couldn’t figure out what were holes and what weren’t, what the bruises meant, the blood spots, the abrasions. The pains in my body were not precise instructions for the future or reliable accounts of the past. The entire upper half hurt: neck arms glands abdomen back eyeballs throat face shoulder head. There was one spot, on the side of what would be my new left breast, that hurt like an emergency. There was another spot, on the side of what would be my new right breast, that hurt like a minor emergency.
In a note about prospective titles for what would become “Illness as Metaphor,” Susan Sontag wrote, “To think only about oneself is to think of death.” Being a writer makes me a servant of sensory details, issuing forth page after page. I am certain that my illness would make a better story if it were someone else’s. Who would want to hear the hammer always complaining about its meeting with the nail? The slightly ill but undiagnosed are better narrators than the truly ill. Their suffering is not so overdetermined. They can be lavishly self-defined, poetic with the glamour of the sick person’s proximity to finality.
To write about oneself may be to write of death, but to write about death is to write of everyone. As Audre Lorde wrote, in “The Cancer Journals,” after she was given a diagnosis of breast cancer, at the age of forty-four, “I carry tattooed upon my heart a list of names of women who did not survive, and there is always a space left for one more, my own.”
After my double mastectomy, I am evicted from the recovery ward. The nurse wakes me up from the anesthesia and attempts to fill out the exit questionnaire while I argue with her that I am not O.K. I tell her that my pain is not managed, that I have not yet gone to the bathroom, that I have not yet been given instructions, that I cannot stand. Then the nurse makes me leave, and I leave.
You can’t drive yourself home, of course, when you are whimpering in pain, unable to use your arms, with four drainage bags hanging from your torso, delirious from anesthesia and barely able to walk. You are not supposed to be alone when you get home, either. But no one really asks how you manage it once you are forced out of the surgical center—who, if anyone, you have to care for you.
Ten days after my surgery, I have to go back to work. I’ve been teaching through the months of chemotherapy, but, despite this, I’ve run out of medical leave. I am driven there by my friends, many of whom have already had to make great sacrifices to help me. Some write checks, some help me drain the surgical tubes stitched to my body, others send mixtapes or cannabis popcorn. My friends carry my books into the classroom, because I can’t use my arms. Delirious from pain, I give a three-hour lecture on Walt Whitman’s poem “The Sleepers”—“wandering and confused, lost to myself, ill-assorted, contradictory”—with the drainage bags stitched to my tightly compressed chest. My students have no idea what has been done to me or how much I hurt.
I have always wanted to write the most beautiful book against beauty. I’d call it “Cyclophosphamide, doxorubicin, paclitaxel, docetaxel, carboplatin, steroids, anti-inflammatories, antipsychotic anti-nausea meds, anti-anxiety anti-nausea meds, antidepressants, sedatives, saline flushes, acid reducers, eye drops, ear drops, numbing creams, alcohol wipes, blood thinners, antihistamines, antibiotics, antifungals, antibacterials, sleep aids, D3, B12, B6, joints and oils and edibles, hydrocodone, oxycodone, fentanyl, morphine, eyebrow pencils, face creams.”
Then the surgeon calls to tell me that, as far as she can tell, the drugs have worked, the cancer is gone. The surgery performed after six months of chemotherapy reveals a “pathologic complete response,” the outcome I’ve hoped for, the one that gives me the greatest chance that, when I die, it won’t be of this.
With that news, I am like a baby being born into the hands of a body made only of the grand debt of love and rage, and if I live another forty-one years to avenge what has happened it still won’t be enough.
I have always hated every shade of the heroic, but that doesn’t mean I’ve never had that look. The common struggle gets pushed through the sieve of what forms we have to describe it, and before you know it the wide and shared suffering of this world is narrowed and gossamer, as thin as silk and looking as special as the language it takes to tell it.
Keenly felt suffering gets assigned to one type—some elegant specialist’s languorous and pale upper-class faintness of being. If you didn’t know me, you might think, too, that my illness was so precious it was merely a suffering for the sake of semiotics. But I was a single mother who had no savings and no partner to care for me, who had to work all through my treatment at a job where I was advised to never let on that I was ill. In other words, my cancer, like almost anyone else’s, was ordinary, as was, apart from my practice of writing, my life.
My cancer was not just a set of sensations or lessons in interpretation or a problem for art, although it was all of these things. My cancer was a captive fear that I would die and leave my daughter in a hard world with no resources, a fear, too, that I had devoted my life to writing and sacrificed all I had and never come to its reward. It was a terror that all I’d ever written would sit data-mined but not read in Google’s servers until even Google’s servers were made of dust, and in the meantime I would become that unspeaking thing, a dead person, leaving too soon everyone and everything I loved the most.
I tell my daughter that my BRCA genetic test came back negative. I tell her that, without a hormonal cause and without a genetic tendency and without obvious life-style factors, the cancer I had probably just came from exposure to radiation or random carcinogens, that she doesn’t have to worry that she is predisposed or genetically cursed. “You forget,” she answers, “that I still have the curse of living in the world that made you sick.”
Despite icing my hands and feet all during chemotherapy, my fingernails and toenails begin to lift from their beds. Fingernails lifting from fingers hurts as badly as fingernails lifting from fingers should. I bandage my iridescently painted nails onto me. I’ve lost friends, lovers, memory, eyelashes, and money, so I am stubbornly opposed to losing anything else to which I am attached. My nails fall off despite my opposition to their loss.
My nerves begin to die, disintegrating into a sizzling sensation from their ends in my fingers, toes, and genitals. My fingers become the most annoying solipsists: numb to the world, outraged in their interiors. The nurses give me a glossy binder with a photo of a smiling silver-haired woman on its cover. The title is “Your Oncology Journey,” and inside it tells me that the solution to my condition, neuropathy, is to ask others to button my shirt, but it doesn’t explain who. I’m made clumsy by altered proprioception, too. I can no longer trust my feet to tell me where I stand.
In the end, my body bore the unbearable, as many of ours do. I think of the medieval Islamic philosopher Avicenna’s floating man, who, denied all sensation, still knows, as proof of the soul, that he exists. I am not sure that I believe him. A better answer is found in the Roman poet Lucretius’ argument in his epic poem De Rerum Natura, that we can die inch by inch. Every cell is a kingdom of both substance and spirit, and any kingdom can be overthrown. Our life force, like our bodies, never seems to issue away from us all at once. Anyone who has been half dead can attest to this. What we call our soul can die in small quantities, just as our bodies can be worn, amputated, and poisoned away, bit by bit.
For a long time while I am sick, I feel as if I am probably dead, haunting the earth’s slightly familiar territory, a traveller to an afterlife that, for whatever reason, I am sometimes allowed to believe is real. If I were still alive, I think, I’d have at least visited California. I read later that feeling like you are dead can be caused by certain kinds of brain damage, such as the kind I’ve endured from chemotherapy. I’m a ghost, but my loss of me isn’t even metaphysical—it’s mechanical. Still, the rational explanation of why I feel dead half the time does little to mediate the irrational horror of existing as if I do not. Here we are, here I am, alone and myself, half of me fallen off, half of us gone.
I know it has all been confusing, or at least it was to me. But it’s the same confusion as when I am confident that every person who has ever lived knows exactly what I mean when I describe feeling like a snake on the path in the dappled sunshine which turns out, on close inspection, only to be a snake’s discarded skin.
To see a snake is also to think of the way a snake slithers out of its skin, the way it has to rub its skin against something hard so that the skin begins to loosen and also the way the snake must generate sufficient new skin so that the old might be left behind. To see a snake is to think of the way the snake’s eyes glaze over and it might not be able to see for a bit because there it is, getting new skin, getting rid of the old, lost in the process of becoming something else.
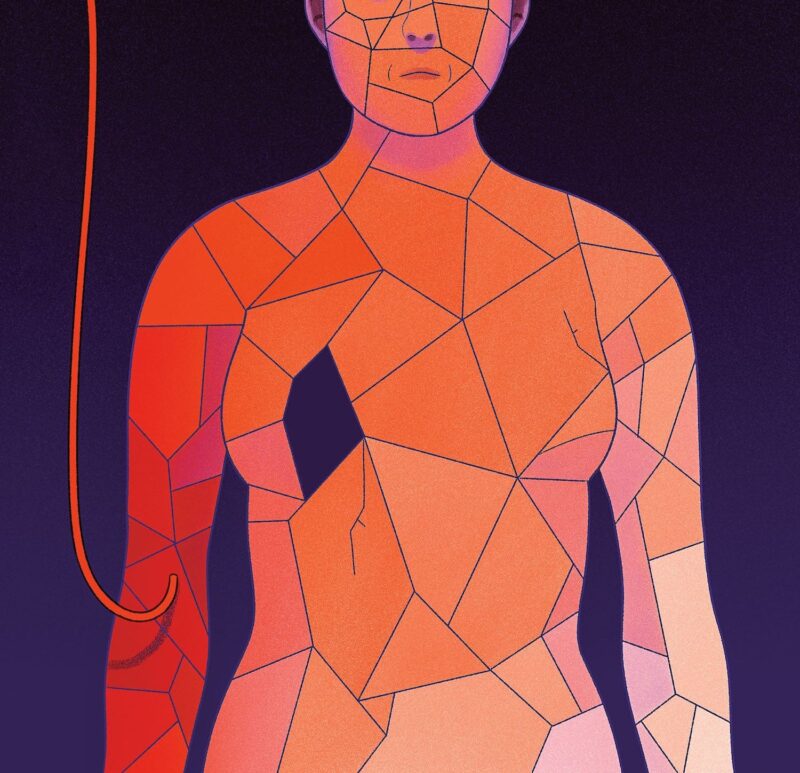
The original article was published in the New Yorker print edition of the April 15, 2019, issue, with the headline “The Undying.” And re-published online recently: https://www.newyorker.com/magazine/2019/04/15/what-cancer-takes-away. From the same story, the author also published The Undying: Pain, Vulnerability, Mortality, Medicine, Art, Time, Dreams, Data, Exhaustion, Cancer, and Care that won the 2020 Pulitzer Prize in the General Nonfiction category. Illustration by: Bianca Bagnarelli.