Interview with Fausto Petrelli, oncology unit, asst Bergamo ovest, Treviglio (Italy).
Q.Steroids are commonly used in patients with solid tumours for supportive therapy. Your systematic review and metanalysis recently published in European Journal of Cancer seems to question the real usefulness of this approach. Why?
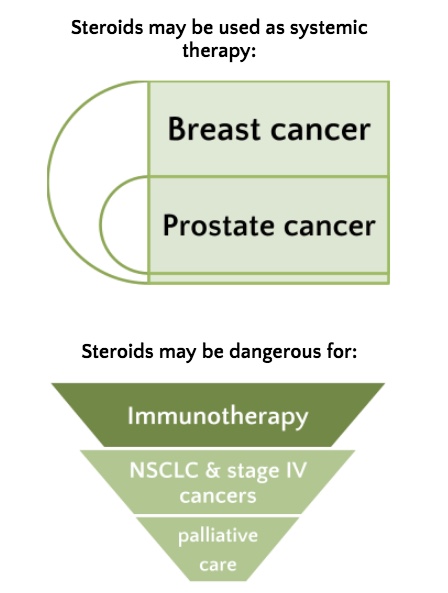
A. Steroids have indoubt beneficial effects in cancer patients in particular for control of symptoms of advanced disease (brain edema, pain, dyspnea, etc) and negative effect on immunity. We found that in setting where they are not used for curative purposes (e.g. prostate cancer), they may exert a detrimental effect on survival. This is now ever more debated in those patients that are undergoing immunotherapy. The main effect on infection risk, diabetes, risk of sepsis, and immunosuppression may explain the reduced survival observed in these patients. All these effects may reduce prognosis, in particular in advanced cancer patients where the immune system is impaired. No data are derived from adjuvant or early settings where they are usually used only for CINV (for pain or during RT) for short periods. Some of the included studies report data on breast cancer where steroids were seldom used many years ago in adjuvant schedules.
Q. Your paper refers to 76 articles from 2057 screened references. How did you select them?
A. We selected prospective or retrospective studies, published in full paper and in the English language, that reported the outcome of cancer patients according to steroid use (any steroids vs no steroids) independent of the aim of therapy (curative or palliative scopes). The main endpoints were overall survival (OS) and progression-free survival (PFS) between steroids user (intervention group) and standard therapy without steroids (comparator group). We excluded case reports and haematological malignancies where corticosteroids are the standard of care for those diseases. We then performed subgroup analysis according to the type of study (retrospective/prospective and randomized studies), the reason for steroid use (e.g., supportive care vs curative scopes), type of disease, stage (early vs advanced), risk of bias (high vs low), and type of analysis (uni vs multivariate).
Q. Based on these data, are you definitely recommending to reduce or even avoid use of steroids in patients with advanced solid tumours?
A. Despite the retrospective nature of most studies, the more important result is the harmful effect of steroids in NSCLCs, in metastatic patients and in the palliative setting. This means that in case of symptoms control, steroid duration should be limited in terms of duration and doses and avoided during immunotherapy, particularly in NSCLC patients. This recommendation, however, is still included in major guidelines that discuss the correct immunotherapy administration and did not derive from this meta-analysis only. For metastatic patients undergoing palliative care, where quality of life is the primary endpoint, steroids are useful and should continue to be used. We suggest that in patients that have stopped active treatment and are on palliative care alone, steroids may be offered for obvious reasons. Conversely, in subjects undergoing active treatments (e.g. chemo and/or immunotherapy), steroids must be used judiciously, only for brief periods, to mitigate chemotherapy’s side effects (delayed or acute CINV), pain or brain oedema due to brain/bone metastases during RT for example.
Q. Your paper has different figures. Which one best synthesises your take home message?
A. I think clinicians may focus on table 2 of our paper, that report subgroups analysis. The message is not alarmist at all. We must continue to use steroids for CINV, such as during RT for brain mets or symptomatic bone metastases. We should identify a little subgroup of patients (for me, NSCLC patients or other solid tumors, in particular, undergoing therapy with immune checkpoint inhibitors where corticosteroids are dangerous. We unfortunately, cannot answer the question about the duration and dose of steroids that could be administered safely. Indeed, a randomized study will not never be designed with this scope. New antiemetic drugs (anti-NK1) permit now to deescalate steroid dosage during CINV prevention. In the meanwhile, based on these results, a cautious policy of steroids use minimization should be pursued by any clinician dealing with cancer patients.