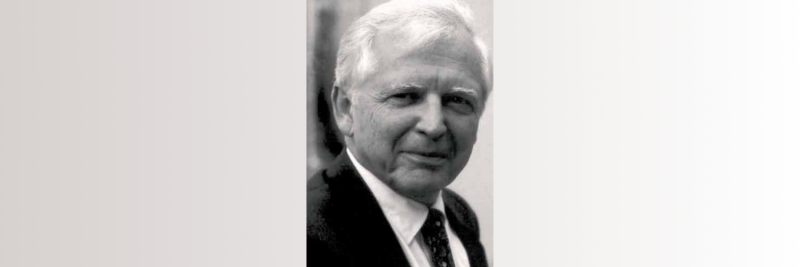
Harald zur Hausen, virologist and Nobel laureate, passed away on May 28th. His great discovery, that cervical cancer is caused by the human papilloma virus (HPV), opened the way for significantly reducing the risk of developing this disease – still the fourth biggest cancer killer of women globally – among upcoming generations the world over.
It also helped challenge fatalistic perceptions of cancer at a popular level, by showing that it is possible to discover what causes it, and to take steps to protect against it. And it opened the way for the World Health Organization to initiate its first global health campaign against cancer (aside from its anti-tobacco work), with a global call issued in May 2018 for action to eliminate cervical cancer.
The goal at the heart of that campaign, 90% of all girls to be fully vaccinated against the HPV virus by age 15, is a direct legacy of scientific research done by Harald zur Hausen, who demonstrated the link between cervical cancer and two subtypes of the human papilloma virus (HPV 16 and 18), initially against the prevailing academic opinion, for which he was awarded the 2008 Nobel prize for Physiology or Medicine. The virus was subsequently found also to be responsible for many cancers of the vagina, vulva, anus and penis, as well as some head and neck cancers.
How it started: Epstein Barr virus in the Henle lab
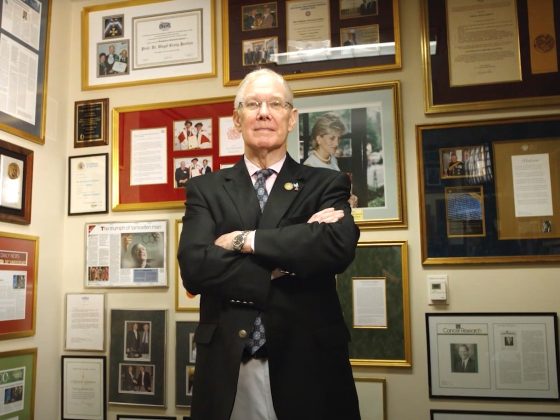
Born in Gelsenkirchen in western Germany in 1936, zur Hausen qualified as a medical doctor at the University of Düsseldorf in 1960. He was particularly interested in the relationship between viral infection and cancer, and moved into research. He trained himself in basic molecular biology laboratory skills, and began exploring whether the vaccina (cowpox) virus could damage DNA in mouse cells. After completing his PhD, he applied to do a postdoc stint at Philadelphia’s Children’s Hospital in the lab of Werner and Gertrude Henle, who were studying the Epstein-Barr virus – also known as human herpes virus 4 – which had been observed in cultured Burkitt lymphoma cells. It was during the course of this work that zur Hausen started to develop the idea that, when infected by a virus, the viral DNA could persist in cells over many years and occasionally become activated, causing modifications of the cell genome which could then lead to cancer.
He returned to Germany to run his own lab at the Institute of Virology in Würzburg. In 1972 he was appointed professor of virology at the University of Erlangen-Nuremberg in Bavaria. By this time, he was doubting the prevailing view that cervical cancer was caused by the herpes virus. ”That was what 95% of the community was thinking,” says Lutz Gissmann, who worked alongside zur Hausen as a PhD student, and went on lead the division Genome Modifications and Carcinogenesis at the German Cancer Research Centre (DKFZ), and is now retired. In general, at that time in the US, there was little interest in pursuing research into the link between viral infection and cancer, as it was not considered particularly significant or worth funding. Those who did support the theory of a viral link to cervical cancer were convinced the offending virus was herpes simplex type 2 – a different subtype of the virus known to cause Burkitt lymphoma.
Zur Hausen didn’t agree. He started to study other viruses, including the HPV virus, which caused skin warts. One of the first discoveries made by Gissmann and zur Hausen was the heterogeneity of the virus – we now know there are more than 100 subtypes. By 1977, when he moved to the Institute of Virology in Freiburg, zur Hausen’s lab had identified DNA from two HPV subtypes in genital warts – but these were not present in cervical cancer biopsies. Persistence paid off, however, and by 1983, when he became director of the German Cancer Research Centre at Heidelberg, zur Hausen’s lab had identified HPV 16 and HPV 18, and could show that the former was present in 50% of cervical cancers and the latter in a further 17–20%. In all, these two strains were shown to be present in 70% of all cervical cancers.
Convincing the sceptics
It took a while to convince his fellow researchers, however. The scientific community were reluctant to accept this paradigm shift, and zur Hausen faced a lot of hostility. Gissmann recalls, in particular, one Herpes Simplex Virus conference where zur Hausen stood up and challenged the dominant narrative and reported on the far stronger evidence he had compiled indicating the HPV virus as the culprit. But most colleagues remained sceptical. It took five to ten years to erode that scepticism, with further evidence of HPV found in cervical cancer biopsies, and with many groups confirming the finding, says Gissmann, which significantly delayed work on developing a vaccine.
Speaking to Cancerworld in 2005, a year before the first HPV vaccine became available, zur Hausen said he had approached companies to create such a vaccine as early as 1984, but the industry were put off by the scientific disagreement and lost interest. “If our original conviction that this virus must be causative had been carried through, we would have made an earlier start,” he noted. It took until 1991, when epidemiological evidence was added to zur Hausen’s genetic evidence, for industry to get the certainty they needed to proceed, with the first HPV vaccine coming on the market in 2006.
As of 2022, 125 countries routinely vaccinate girls for HPV and 47 countries also vaccinate boys.
In 2008 zur Hausen was awarded the Nobel Prize in Physiology or Medicine for his discovery of human papilloma viruses causing cervical cancer.
Infections and cancer: a lifelong interest
Zur Hausen retired in 2003, but he continued to probe how infection can cause cancer for the rest of his life, working with his wife, virologist Ethel-Michele de Villiers. In 2019, with molecular biologist Timo Bund, they published a study connecting new infectious agents found in beef and cow’s milk to a higher risk of developing colon and breast cancer. Known as ’Bovine Meat and Milk Factors’ (BMMFs), these DNA molecules infect cattle and contain sequences similar to the genes found in viruses, that allow them to replicate. Zur Hausen and his co-authors hypothesised that, rather than red meat itself, it is these pathogens that can trigger cancer in colon and breast tissue, decades after infection.
Clearly zur Hausen felt his work was not done and believed there is still much more to learn – a point he made in the concluding remarks of his 2008 Nobel Lecture: “Research on infectious causes of human cancers has great potential for future surprises.”