Offering ‘stop smoking’ support as part of a national lung cancer screening programme resulted in nearly nine out of ten people agreeing to an immediate consultation and three-quarters accepting longer term support. The evaluation of an ‘opt-out’ face-to-face smoking cessation service located at a community based mobile screening unit, published in The European Respiratory Journal, April 18, found one in seven of eligible participants reported still not smoking four weeks later.
“Offering sufficiently funded, integrated, stop smoking interventions, which are provided as a routine component of lung cancer screening, results in high uptake across a range of demographics and therefore offers a very real opportunity to reduce smoking related health inequalities,” Rachael Murray, the corresponding author, from University of Nottingham, tells Cancerworld.
Low-dose computed tomography (LDCT) screening for lung cancer has been shown in a number of studies to reduce lung-cancer-specific mortality. However, up to half of people attending cancer screening are current smokers, and offering them support to quit at the time of attendance presents an ideal opportunity to maximise their chance of successful quitting.
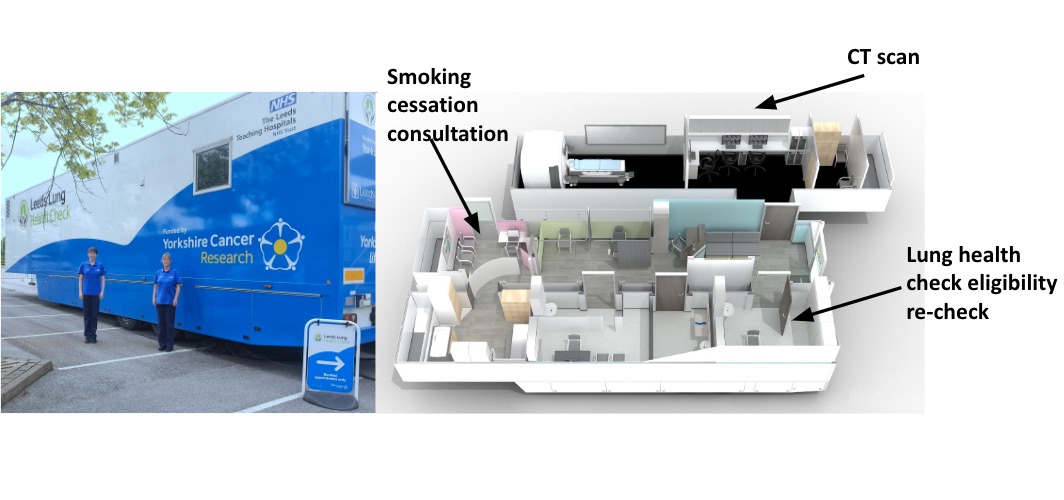
The potential utility of delivering an opt-out smoking cessation support package as part of a community-based lung cancer screening trial was investigated within the Yorkshire Lung Screening Trial (YLST). LDCT screening took place in mobile units located in convenient community-based locations, with smoking cessation interventions offered to all consenting individuals who underwent an LDCT scan and who had smoked in the last month or had an exhaled carbon monoxide reading ≥6 ppm. Smoking cessation support consisted of an immediate session of behavioural support delivered face-to-face at the time of the Lung Health Check and direct provision of quit aids (such as nicotine replacement therapy, e-cigarettes, or a GP prescription for varenicline or bupropion).
All eligible participants engaging with stop smoking support were contacted by phone four weeks after their screening visit to answer questions relating to their smoking status, with optional carbon monoxide test validation if they reported quitting. “We wanted this research to replicate the ‘real world’ as far as possible. Stop smoking support was presented as part of the standard care package, not an additional component or a research project, which would have biased uptake and engagement. Our approach also means that findings are immediately generalisable to the targeted Lung Health Check programme,” says Murray.
Results showed that, of 2,150 participants approached who were current smokers, 1,905 (89%) accepted the offer of a smoking cessation consultation during the initial visit, of whom 1,609 (75%) received ongoing smoking cessation support over subsequent weeks.
Overall, 323 people (15% of all those attending screening eligible for stop smoking support) reported not smoking at four weeks, with 266 of these (12.4%) providing a breath sample verifying (by exhaled carbon monoxide) that they had stopped.
For those accepting ongoing smoking cessation support, 24% opted for nicotine replacement therapy alone, 18% an e-cigarette alone, and 33% a combination of both. Pharmacotherapy was selected for 7% of participants, no support was accepted by 14%, and data were missing for 4%.
Uptake of ongoing support was not associated with age, ethnicity, deprivation, or educational level in multivariable analyses, although men were found to be less likely to engage [adjusted OR (ORadj) 0.71, 95%CI 0.56–0.89]. Uptake was higher in those with higher nicotine dependency, motivation to stop smoking, and self-efficacy for quitting (an individual’s belief in their ability to successfully quit).
Multivariable analyses of smokers attempting to quit suggested four-week quitting was more likely in men (ORadj 1.43, 95%CI 1.11–1.84), and in those with higher motivation to quit and previous quit attempts, while those smoking more cigarettes a day were less likely to quit.
“With 2,150 eligible participants attending for lung cancer screening and continuing to smoke, this study is the largest to report uptake and outcomes from an opt-out face-to-face smoking cessation service co-located with a community-based mobile screening unit,” write the authors. “Furthermore, the comprehensive analysis of demographic, clinical and behavioural parameters allows a thorough characterisation of the factors associated with uptake of smoking cessation support and 4-week quit rate,” they add.
The finding that participants with higher levels of nicotine dependency were more likely to engage with smoking cessation support surprised the authors. “This might be due to the opt-out nature of the intervention, coupled with the teachable moment of attendance at lung screening encouraging those people who would not proactively seek quitting support to take advantage of this offer,” write the authors.
The differences between male and female smokers participating in lung cancer screening with respect to uptake of smoking cessation support and successful quitting outcomes, they write, requires further research. “Females tend to be more likely to engage with an offer of stop smoking support, whereas males are more likely to attempt to ‘go it alone’. Despite this, it is commonly accepted that males typically find it easier to quit smoking than women,” says Murray. The reason, she adds, is that women tend to experience more severe withdrawal symptoms than men, and there is also a theory that nicotine blocks the production of oestrogen.
The authors provide a message to health funders to make protected funding available to integrate stop smoking support as part of the lung cancer screening package. “An initial consultation and provision of quit aids should be available either immediately or in very quick succession to the lung screening appointment, to capitalise on the receptiveness of attendees to consider behavioural change activities,” says Murray. “Further, future interactions should be seamless, to avoid a loss of engagement that occurs when individuals pass between fragmented services.”
The team also undertook a ‘complete process evaluation’, which will be published later, involving interviews with trial participants and smoking cessation advisors at a variety of time points to understand their views on the stop smoking support offered. They plan to conduct further research to describe optimal ways of providing stop smoking support that are both effective and practical in real world settings. “There remains much work to do to identify how best to engage those who choose not to accept the support offered and optimise the opportunity presented by combining these lifesaving interventions,” says Murray.
In an accompanying editorial, Keir Lewis, from the University of Swansea, writes that the study builds on the established smoking cessation principle of the ‘teachable moment’. “This takes practical advantage of the personal teachable moment, utilises precious time and impresses on the smoker the urgency of quitting,” he writes. Answering the rhetorical question of why the study was important, Lewis writes. “It is ambitious in aiming to embed two services in real-time, but also a very pragmatic piece of work, designed specifically to replicate standard of care: the initial invites made no reference to the fact that the study was a research project, but instead presented it as routine care.”
Cancerworld reported on an earlier step in this research – the Yorkshire Enhanced Stop Smoking study – back in 2021, as part of an article looking at ways to improve the risk-benefit of lung screening programmes through improving targeting and impact.