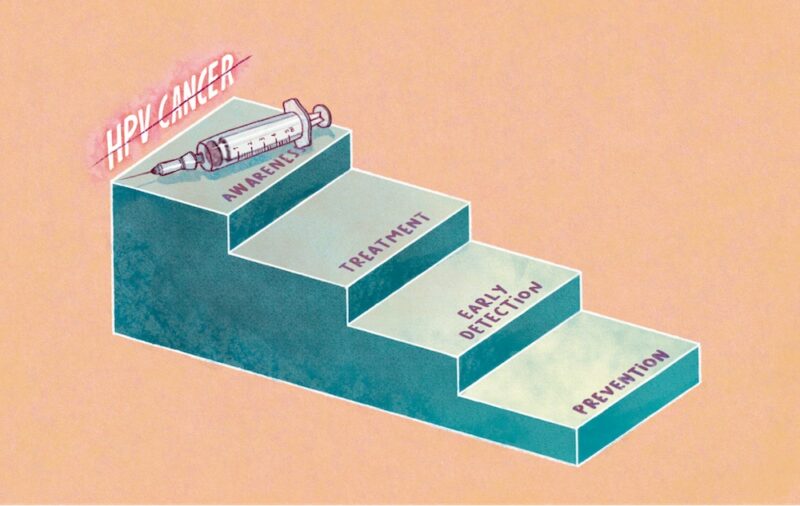
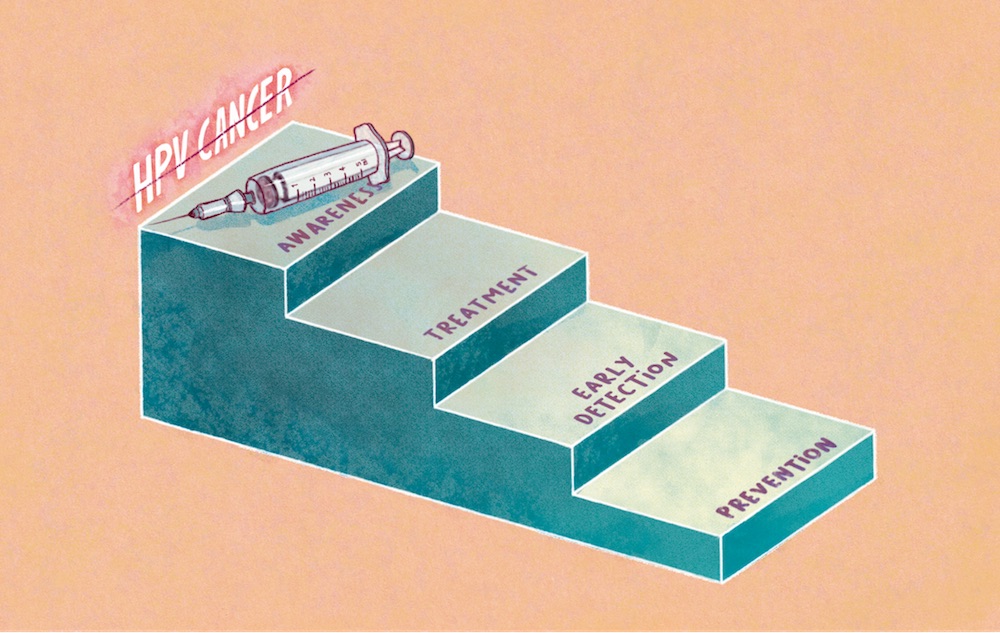
A new report underlines that vaccination, screening, treatment and public awareness, provide the cornerstone for eliminating cancers linked to the human papillomavirus (HPV) in Europe. The report was published by The European Cancer Organisation, Brussels on 7th October. The report, ‘Viral Protection: Achieving the Possible’ details a four step plan that calls for urgent action to eliminate the 87,000 cancer cases caused by HPV in the WHO European Region each year.
“Action across the European region to eliminate the cancers and diseases caused by HPV has the potential to save hundreds of thousands of lives and improve the quality of life of many more,” write the authors, who are members of the European Cancer Organisation’s HPV Action Network. The network was launched in December 2019 following resolutions passed at the 2019 European Cancer Summit to implement strategies to eliminate cancers caused by HPV in all European countries by 2030.
HPV is a common sexually transmitted infection that is responsible for almost 5% of all cancers worldwide. The virus is best-known for causing cervical cancer, but also causes anal, penile, vaginal, vulval, and oropharyngeal cancers. It is estimated that around 85−90% of sexually active women and men will acquire HPV at some point in their lives, with 12 or so of the 200 HPV infection types associated with development of cancer. However, diseases caused by HPV can be prevented through vaccination.
The new report, representing the first Europe-wide advocacy initiative to tackle HPV-caused cancers, highlights major areas for concern including:
- That 26% (14 out of 54) of countries across the WHO European region have yet to introduce national HPV vaccination programmes for girls. This decline is due to a variety of reasons including cost, restricted access to health services, concerns about vaccine safety and lack of service co-ordination.
- Only 48% of countries (n=26) vaccinate or have made a commitment to start vaccinating boys (as well as girls) against HPV.
- Few countries meet the widely-accepted target of 80% HPV vaccination coverage.
- 16 countries continue to have ‘opportunistic’ cervical cancer screening, as opposed to population-based screening where invitations are systematically issued. The consequence is that success depends on the initiative of individual women and their doctors, resulting in lower uptakes.
- Treatment outcomes vary widely across European countries, with 5-year survival rates for cervical cancer ranging from highs of 80% to lows of 54%.
- Fears around HPV vaccine safety, fuelled by ‘fake news’ have resulted in falls in vaccine uptakes. For example, uptake of HPV vaccination in Denmark fell from 90% for girls born in the period 1998−2000 to 54% for girls born in 2003.
- The COVID-19 pandemic has significantly disrupted HPV vaccination programmes across Europe and (at least in the short-term) will undoubtedly cause a dip in vaccine uptakes.
The report calls for urgent evidence-based policy and practical action by the EU and all governments throughout WHO European region, to eliminate cancers and diseases caused by HPV, with goals identified including four action areas:
- HPV prevention via gender neutral vaccination programmes. Universal (‘gender-neutral’) HPV vaccination for all adolescents and optimal levels of uptake.
- Early detection by HPV testing. Cervical cancer screening programmes using HPV testing technology since it is much more accurate than the traditional Pap smear. Currently, no screening programmes are available for any of the other HPV-caused cancers.
- Getting better on HPV Cancer Treatment. Cancer treatments must be consistently and equitably offered across all European countries in line with best practice guidelines and care and support to maximise patient quality of life.
- Raise public and professional awareness about HPV to improve vaccination and screening uptakes. Recent research suggests that only 73% of people in Northern Europe believe vaccines to be safe in a general sense.
“The new report … sets out how elimination of cancers and diseases caused by HPV can be realised through realistic investment and most importantly by building on good practice already in place in many but still too few European countries,” says Matti Aapro, President of the European Cancer Organisation.
The report highlights the European Commission’s ‘Beating Cancer Plan’, due for publication later this year, as an opening to make HPV cancer elimination a formal European shared goal.
“The forthcoming Beating Cancer Plan is a unique opportunity for the EU to take the lead in eliminating all cancers caused by HPV in men and women,” says Daniel Kelly, co-chair of the HPV Action Network. “We urge the Commission to adopt our proposals for action and for member states to act, especially those currently behind in terms of HPV vaccination, screening, treatment and public awareness.”