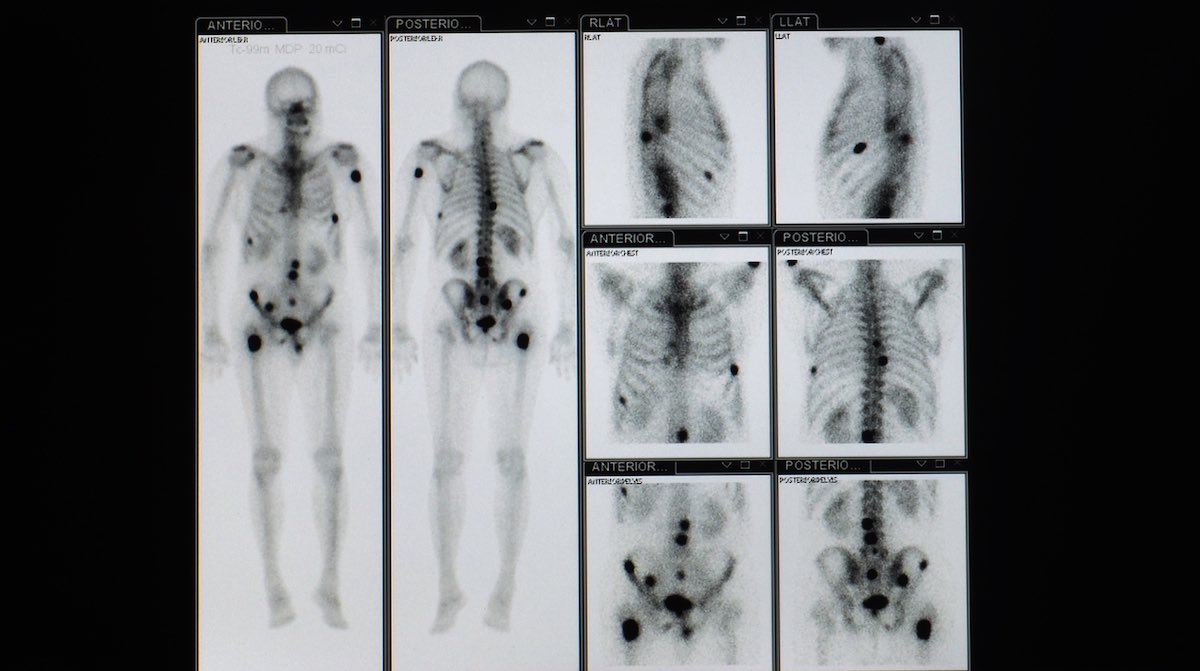
Treating high-risk, asymptomatic bone metastases with prophylactic radiation therapy reduces painful complications and extends overall survival. The study, abstract LBA 04, presented at the American Society for Radiation Oncology (ASTRO) Annual Meeting, held October 23–26, 2022, in San Diego, California, demonstrated that radiotherapy reduces skeletal-related events and hospitalisations for skeletal-related events.
“This first randomized trial of its kind suggests radiation for high-risk bone metastases in patients without pain may be a promising new treatment approach,” said study presenter, Erin Gillespie, a radiation oncologist from Memorial Sloan Kettering Cancer Center, New York.
Historically, palliative radiotherapy has focused on reducing existing pain and other symptoms when cancer is no longer considered curable. Radiotherapy has not been used for asymptomatic metastases outside the oligometastatic setting (where limited metastases are treated with local ablative therapy). Patients remain on systemic therapy until lesions become symptomatic, when they are offered radiotherapy. Inspiration for the current study came from observations that up to 60% of patients have evidence of lesions visible on prior imaging. This ‘potential window’ for intervention prompted Gillespie and colleagues to design a trial to explore whether radiotherapy applied to lesions before they become painful can prevent complications and improve patient quality of life.
For the phase II study, between May 2018 and August 2021 investigators identified 78 adults with metastatic solid tumours and ≥5 metastatic lesions, including at least one asymptomatic high-risk bone lesion. Whether a lesion was considered high-risk or not was determined by size (≥2cm in longest diameter), location in the junctional spine, disease involving the hip or sacroiliac joint, and whether located in the long bones of the body. The primary cancer types of patients in the study were lung (27%), breast (24%), and prostate (22%).
Participants were randomised 1:1 to receive standard of care treatment (including chemotherapeutics, targeted therapies, immunomodulatory agents, and hormonal therapies; n=39) or prophylactic radiotherapy with no restrictions on initiating systemic agents (n=39). Data was evaluable on 35 patients (with 62 high-risk bone lesions) in the radiotherapy arm and 36 patients (with 49 high risk bone lesions) in the control arm.
Results at the end of one year showed skeletal-related events (including pain, fractures and compression of the spinal cord requiring surgery or radiotherapy) occurred in 1.6% (1 out of 62 lesions) in the radiotherapy arm versus 29% (14 out of 49 lesions) in the standard of care arm (P<0.001).
No patients were hospitalised for skeletal-related events in the radiotherapy arm compared with 11% (4 patients) in the standard-of-care arm (P=0.045), and the radiotherapy arm showed significant improvement in Brief Pain Inventory scores (P=0.039).
Median overall survival was 1.7 years in the radiotherapy arm versus 1 year in the standard of care arm (HR=0.5; 95%CI 0.28–0.91, P=0.02).
“It is thought-provoking that radiation to prevent pain could potentially prolong life. It suggests that treating to cure the cancer is not the only thing that can help people live longer,” said Gillespie.
The overall survival difference, she added, had not been expected, but there was a rational explanation, with previous studies demonstrating that palliative care can extend survival.
Due to the small size of the study, the results could be considered “hypothesis-generating”, said Gillespie, and require a larger study to replicate the findings. Many questions remain, including how to identify patients with metastatic lesions, at what point would patients with metastatic lesions benefit from radiotherapy, and how to identify those lesions that are most likely to become problematic? “From the other perspective, only 30% of patients had events so there is the question of potentially over treating patients who don’t go on to have events and whether they all need radiation?” said Gillespie.
Commenting on the study, Shankar Siva, an independent investigator, from Peter MacCallum Cancer Centre, Victoria, Australia, told Cancerworld, “This study moves the needle forward. In my opinion it’s likely to change practice. It’s a very reasonable conclusion that earlier radiotherapy is better; it’s somewhat akin to throwing a life vest out to someone who looks in trouble in the water rather than waiting for them to drown.” The surprising finding, he added, was that early intervention with radiotherapy improved patient longevity. “This finding warrants confirmation in a larger randomised phase III trial,” said Siva.