Earlier cancer diagnosis could make a huge difference to cancer survival rates – only two in ten of those diagnosed after their cancer has metastasised survive, compared with nine in ten diagnosed when the disease is still localised. In 2020 the UK National Health Service announced a partnership with US biotech GRAIL to tackle the problem, conducting a trial of their multi-cancer early detection liquid biopsy ‘Galleri’ that involved 140,000 people.
Galleri is one of the first blood tests able to reliably detect ‘cell-free’ fragments of DNA originating from tumour sites, and provide an early warning for the presence of multiple types of cancer in asymptomatic individuals. The hope is that this will usher in a new era of screening for multiple cancers, beyond those already screened for. But there are still many questions, including how these tests should best be used, and how they will affect people’s chances of surviving cancer in the real world.
“We currently have screening programmes in the UK which involve lung, bowel, breast, cervical, but actually, many different cancer types do not have screening programmes like pancreatic, ovarian, head and neck,” comments Oxford University Hospitals medical oncologist Lennard Lee, who is also the NHS England project lead for multi-cancer early diagnostics. The harder-to-diagnose cancers, as well as other cancers that occur at a prevalence too low to make conventional screening an economical option, are often not detected until the later stages. “Multi-cancer early diagnostic tests could provide the answer here,” says Lee.
The NHS-Galleri randomised study of people aged 50–77 with no signs of cancer will test this proposition for 50 types of cancer, reporting results in 2024 after three cycles of annual scan. If successful, the NHS in England plans to roll out the test to a further one million people in 2024 and 2025. “We are probably the first healthcare system to be doing this routinely in our hospitals,” says Lee.
From diagnostics and monitoring to screening and early detection
Liquid biopsies, or blood tests for cancer, are not completely new. Niche tests that detect specific mutations post-diagnosis have been gaining regulatory approval in the last decade, such as the recently approved Guardant360 CDx and FoundationOne Liquid CDx tests. Many of these take advantage of cell-free DNA (cfDNA) – nucleic acid fragments that end up in the bloodstream when cells disintegrate, and can circulate for a few hours before being cleaned up by white blood cells. But the problem in using cfDNA to find tumour mutations has been its low concentrations, which can be as little as one tumour cfDNA fragment among thousands of normal fragments.
Several breakthroughs are now making multi-cancer early detection tests a reality. The first of these is the ability to detect DNA methylation patterns using next-generation sequencing. The addition of methyl groups to DNA is one of the ways that genes can be turned on or off. Nearly 30 million methylation sites exist across the human genome, and changes in these methylation patterns are characteristically found in cancer cells. The large number of methylation sites – more than 1,000,000 can be analysed by GRAIL – makes this much easier to detect than looking for a specific tumour mutation. The second key breakthrough has been the development of machine learning and its ability to use data sets to train itself to identify pattens of methylation for specific cancers.
Galleri uses methylation analysis to look for a cancer signal shared across more than 50 types of cancer
GRAIL, a San Francisco biotech that was spun out, and then reacquired, by Illumina – the global leaders in next generation sequencing – is not surprisingly making use of both these breakthrough technologies. The company does not operate in the European Union, due to prohibitions based on EU merger regulations, but since 2021 its Galleri test has been marketed to individuals in the US at a cost of $949.
The Galleri test uses methylation analysis to look for a cancer signal shared across more than 50 types of cancer, and predicts the tissue or organ where the cancer signal originated. The clinical development programme includes studies covering data from more than 300,000 participants. Eight clinical trials have either published results or are ongoing.
Their 2022 publication compared 10 different machine-learning systems trained on the same samples, each looking at slightly different genomic features. They concluded that, while analysing single nucleotide variants could provide the highest signal sensitivity for cancer (i.e. will be most effective at picking up true cancers), looking at whole-genome methylation best predicts the site of a cancer, making it the most promising technology for multi-cancer early detection.
Alternative tests and technologies: pros, cons and trade-offs
GRAIL are not the only company developing multi-cancer early detection liquid biopsies. In January 2023, the FDA granted breakthrough device designation to the OverC Multi-cancer detection blood test from US biotech Burning Rock. It also uses cfDNA methylation patterns and is designed to detect oesophageal, liver, lung, ovarian and pancreatic cancers in adults aged 50 to 75 with average risk. California-based Singlera Genomics are developing a similar test, PanSeer, and have reported results from a large study in China which was able to detect five different cancers up to four years in advance of diagnosis in a number of individuals.
While these results are promising, one crucial issue for any screening programme is the likelihood that the test will produce false-positives (erroneously indicate a cancer is present, when it is not) or will lead to over-diagnosis and unnecessary treatments. “They are quite similar problems,” comments Francesco Gatto, who is developing novel cancer diagnostic approaches with oncologists at the Karolinska Institute, in Stockholm. While Gatto recognises that current screening programmes in breast, colorectal and cervical cancer save lives, he says there have been “opposite scenarios,” such as with the thyroid cancer screening in South Korea in the early 2000s. “I think most people would agree [it was a] disastrous initiative, because it just flooded the system with a lot of non-lethal thyroid cancers and many people had their thyroid cut out for probably no reason,” he says.
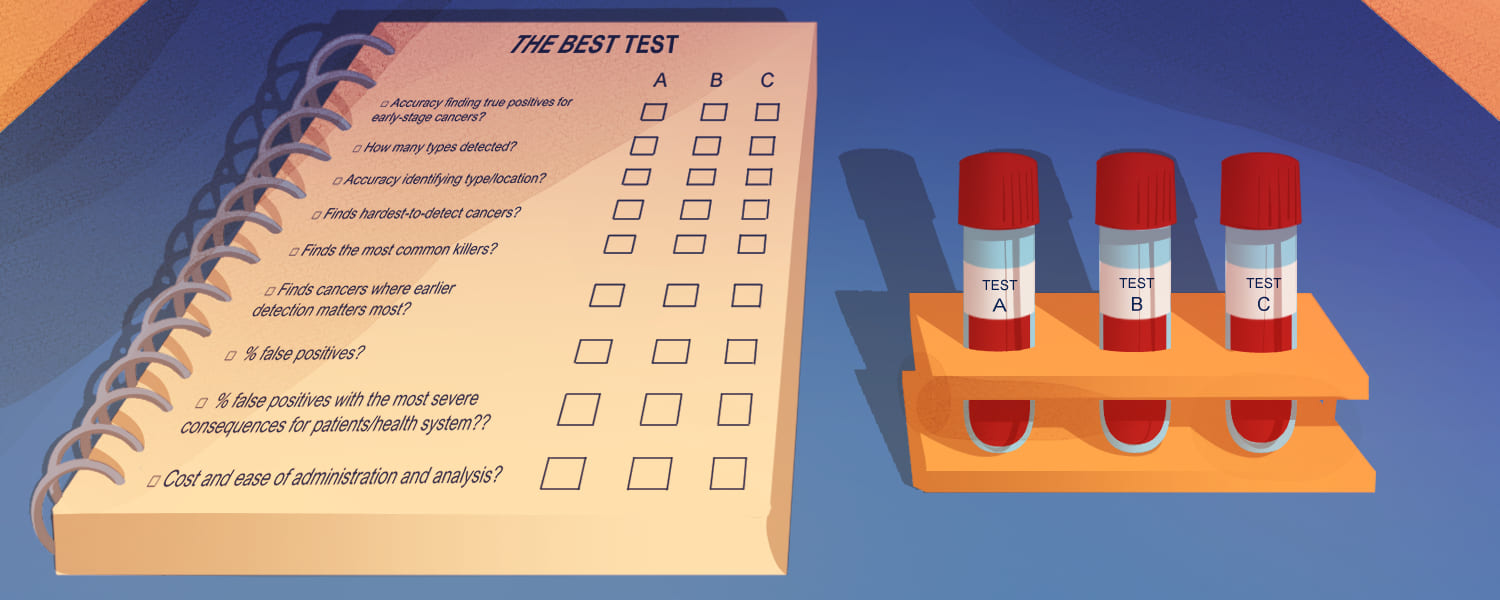
It’s clearly then important to understand both the sensitivity and the specificity of the test – the former being an indication of how far the test can be relied on to show positive when a cancer genuinely is present, and the latter an indication of how far it can be relied on to not give a positive test result when no cancer is present. These factors tend to be related, with higher specificity often leading to a decline in sensitivity and vice versa. GRAIL have said their test gives a specificity of 99.5% with a sensitivity of 76.3% in cancers that cause two-thirds of cancer deaths in the US although, for mass screening programmes, a rate of 1% may still represent a very large number of people.
The company predict that their test, added to current US breast, lung, colon and cervical cancer screening for individuals aged 50–79 years, could detect 615,000 cancer cases, compared with 150,000 from standard screening alone. It would be expected to generate an additional 640,000 false positives, but they say that this represents only 7% more false alarms compared to four times as many cancer diagnoses. They also boldly predict that such testing could reduce all-cancer mortality by a massive 25%. “It’s a very significant impact,” but at the moment, “it’s all purely speculative,” says Gatto.
It’s important to understand both the sensitivity and the specificity of a test… higher specificity often leads to a decline in sensitivity and vice versa
Not all multi-cancer early detection tests focus exclusively on methylation patterns. CancerSEEK, developed at Johns Hopkins University, and now licensed to Exact Science, simultaneously detects the presence of mutations at 201 genomic positions across 16 genes in addition to seeking protein biomarkers using immunoassays. The test came from a collaboration between pancreatic cancer specialist at Johns Hopkins, Anne Marie Lennon, and her colleagues Bert Vogelstein and Nick Papadopoulos, who were working on circulating tumour DNA. “When we looked at it, we found that it alone would not be sensitive enough to detect, so we came up with the concept of combining other markers,” says Lennon. Together, these markers are able to detect breast, colorectal, gastric, liver, lung, oesophageal, ovarian and pancreatic cancers, which account for 60% of all cancer-related deaths.
Their first study, of 1,005 patients, showed sensitivities ranging from 69% to 98% for the detection of five of the cancer types (ovary, liver, stomach, pancreas, and oesophagus), for which there are no current screening tests. Only 7 of 812 healthy controls gave a false-positive, giving a specificity greater than 99%. With such a high specificity your sensitivity drops admits Lennon, “but you need that in a screening test.”
One issue with CancerSEEK has been its difficulty in detecting where the cancer is located – even using machine learning to interpret results, an exact organ could be pin-pointed only 63% of the time. So the team followed up their initial study with a larger real-life prospective study of 10,006 women aged between 65 and 75, with no history of cancer, where positive tests were combined with a PET-CT scan. “We found it works,” says Lennon. “Does it detect every cancer? No, but it does work!” Of the cohort, 26 cancers were detected from the liquid biopsy. Fifteen of those 26 were then followed by PET-CT scans (the other 11 having already developed symptoms that precipitated diagnosis by alternative methods), leading to 9 curative surgeries. Lennon adds that the number of false-positive results was incredibly low, and that only 0.22% of the women underwent an unnecessary invasive diagnostic procedure as a consequence of a false-positive. There were, however, a small number of patients with positive tests who showed no signs of cancer on PET-CT scans. The team are following these patients to see whether the test was correctly detecting preliminary signs of cancer, or whether those results are genuine false-positives.
A metabolic approach to cancer screening
Gatto has been developing another approach to multi-cancer early detection, based not on DNA or proteins, but on metabolic markers, and specifically individual glycosaminoglycan profiles (GAGomes). Glycosaminoglycans are long-chain sugar molecules, often found on cell-surfaces and involved in cell signalling, growth and proliferation. “Our approach [looks at] the last layer in the information of a cell… it detects cancer where methylation assays seem to fail,” he says. Analysing these sugars from plasma and urine samples, using machine learning algorithms, they have been able to identify diagnostic patterns for 14 cancer types.
In their first validation study, using samples from 1,260 cancer patients or healthy subjects, they detected cancer with up to 62% sensitivity, including stage I disease, with 95% specificity, and predicted the cancer location with 89% accuracy. “Of course, we need a lot more data before we can make any claim around [diagnosing] cancer,” admits Gatto, but he thinks what’s exciting about this method is its ability to increase the sensitivity to stage I cancers compared to other, genomic, methods.
This is an important issue for multi-cancer screening tests. To significantly reduce mortality, cancer must be detected at the earliest stages, before metastatic disease develops. “If we have a stage IV cancer, even if we detect it earlier, the survival benefits for the patient will be marginal,” says Gatto. To get real survival benefits the detection needs to be shifted to stages 1 or 2. This is an area where he feels metabolic tests have the edge over genetic tests. According to Lee, who has been working with the cfDNA-based NHS-Galleri trials, early data suggests, perhaps not surprisingly, that the test is at its most sensitive where the cancer is growing very rapidly.
What’s exciting about this method is its ability to increase the sensitivity to stage I cancers compared to other, genomic, methods
Gatto argues that this will likely mean that genomic tests are less sensitive to early disease stages, which he says in borne out by the data. They capture only 10–17% of all cancers at stage I (Science 2020, 369(6499); Ann Oncol 2021, 32:1167–77), compared to around 21–23% with GAGome profiling. “That’s a huge improvement already,” says Gatto, but they hope ultimately to be able to reach 30%.
The reason metabolomic data shows less variation between stages, argues Gatto, is because it is not reliant on detecting DNA, but detects wider cellular changes. With better detection at the earliest stages, Gatto hopes to show a significant impact on survival.
Lennon says CancerSEEK’s combined genetic and protein biomarker approach is already starting to show it can make a survival difference too. The team plan to publish an analysis of the four years of data they have collected within the coming year, but she says already “it looks good.”
Taking one cancer at a time: one set of detection markers may not fit all
Most developers of multi-cancer early detection tests are hoping to facilitate population-wide screening programmes, but DXCover, a clinical-stage liquid biopsy company based in Glasgow, which spun off from the University of Strathclyde, is starting in a different direction. “We’re going to approach it first in the symptomatic population,” says CEO, Mark Hegarty. “We will take it forward, building up cancer by cancer, [so that] you can definitely work out all the health economics.” Hegarty says even testing symptomatic patients could have a big impact. “Sixty percent of the cases that are eventually diagnosed have been cases which have turned up at their primary care practitioner [who] doesn’t have a clue what’s wrong with the patient to begin with.”
“We don’t focus only on information coming from the tumour… We look at the entire information that’s available”
The company has pioneered an approach using infra-red spectroscopy, resulting in unique cancer signatures, established using machine learning. “We don’t focus [only] on information coming from the tumour, like all the genetic approaches, or specific biomarker approaches. We look at the entire information that’s available,” says CTO Matthew Baker. This means that, even in pre-cancerous stages, they can pick up information from a patient’s response to these changes. “Because we’re looking at everything, all of the molecules within human blood, we are able to detect that immune response, as well as anything that is shed from the tumour within our spectroscopic signature,” says Baker.
DXCover have started looking at brain cancers, which are amongst the most difficult to diagnose early. They release very little DNA into the blood stream, making them a poor target for genetic screening. The signatures used by DXCover for detecting brain cancers are based instead on changes in the spectroscopic signals coming from proteins and lipids. The company has completed a clinical validation study, for which they prospectively collected and analysed blood serum samples from 603 patients who either had non-specific symptoms that could be indicative of a brain tumour, or a new brain tumour diagnosis. The test results was compared against the reported diagnosis confirmed via CT brain imaging. Using a model tuned for high sensitivity, the test was able to predict the presence of glioblastoma, the most common and aggressive brain tumour, with 100% sensitivity, and all brain tumours with 96% sensitivity, with a 45% specificity. When tuned for a higher specificity, the model yielded a sensitivity of 47% with 90% specificity.
Baker says that, by carefully selecting different signatures at each stage of the disease, they are able to detect at similar sensitivities and specificities across all stages, and they can improve on the stage I detection of tests like GRAIL’s Galleri, although he says, a comparison has not been made using the same data sets. A larger-scale trial of 2,094 patients, to detect and identify brain, breast, colorectal, kidney, lung, ovary, pancreas and prostate cancer, achieved 61% specificity when tuned to achieve a sensitivity of 93% for stage 1 cancers. The company is now planning a multi-centre study for brain cancer and is also developing a test for colorectal cancer. They hope to gain approval in Europe for their first test by 2025.
While their technology could be developed for a combined test, rather than individual cancer diagnostics, Hegarty says “The jury seems to be out for now [as to] whether there really is going to be proper clinical utility and cost-effectiveness for a multi-cancer early detection test.” One method may not be best for all types of cancers. “We need layers of information” agrees Gatto. He shares the concern that one type of diagnostic marker might not be the optimal solution, and would end up missing some cancers.
False-positives could be a major stumbling block
Concern over the impact of high false-positive rates are still the biggest worry, however, and Hegarty argues that it is not yet clear if this can be controlled. Gatto says the literature generally agrees that a 1% rate of false-positives would be acceptable, but this represents a high number of false-positives for each true-positive. “The equivalent will be for every person that you find with cancer, you will probably find four or five [false positives] without the cancer.” This will mean that people being tested must be very clear about how the test results should be interpreted, he says: a positive test still means that there is a 70–80% probability that the individual doesn’t have cancer. “But of course, it’s very hard to communicate this to people… we will need to engage patient advocacy groups and healthcare payers,” says Gatto.
The consequences of false-positives will also differ for each cancer – a false-positive for pancreatic cancer could mean surgery, but for colorectal just an additional colonoscopy. “The performance characteristics for your test depends upon what test is coming next, as well as where in that pathway you are,” Baker explains. Currently he says there is a push towards very high specificity, to reduce false-positives, but when you are talking about high-risk cancers, or patients with some symptoms, that may not always be appropriate. “For instance, for brain, we think an incredibly high sensitivity is needed, because the next step is a specific medical imaging test… it’s in the patient’s interest to have a higher level of false-positives than is normally acceptable. So I think it really depends upon the application.”
“People being tested must be very clear about how results should be interpreted”
The very different diagnostic pathways and different prognoses for cancers is going to be one of the major challenges for designing multi-cancer screening approaches and tuning levels of false-positives and negatives. Deciding the correct sensitivity and selectivity may also depend on individual patients “One of the questions for the future is, if you’ve got somebody who’s got a higher risk of [cancer], for example they’ve got a very strong family history of colon cancer or pancreatic cancer, then could you change [how these are set]?” asks Lennon.
Other questions for the future will be the age at which screening starts and stops, and how often it is done: “Would you do it every year, every three years, [or] every five years… the data just isn’t there [yet],” says Lennon, “There’s of course unanswered questions, as there always are with new technology… but I think it’s an enormous step forward.” Gatto agrees: “The only way to go,” he argues, is multi-cancer early detection screening for all, backed by healthcare providers. “It’s absolutely critical that this becomes an equitable, widespread programme.”
The prospect of earlier, life-saving diagnoses through multi-cancer early detection screening is certainly a tantalising prospect for oncologists like Lennon, a specialist in pancreatic cancer, which currently has a five-year survival rate of only 8% in Europe. “There’s nothing worse as a physician than having to go in with the patient, pull the blind for privacy, and then sit down with them and their family and tell them, ‘I’m so sorry, you have cancer’,” says Lennon, “so for me, I think that this is wonderful.”
Footnote:
The original version of this article incorrectly gave 100,000 as the number of methylation sites analysed by Galleri – 100,000 refers to the number distinct regions of methylation. It has also been updated to reflect the full extent of studies carried out by GRAIL at the time of publication, and to clarify the diagnostic information that can be inferred from the test, and the data on sensitivity.
Illustration by: Alessandra Superina











1 comment
A very informative, balanced view on liquid biopsies that warns about “running before walking”. Hopeful for cancer patients.
Comments are closed.