What progress can we point to? In Africa, there is a growing awareness of cancers, not just among the healthcare professionals but also communities. This has been largely due to grassroots advocacy – people who were cancer champions coming out and saying: “Listen I had cancer, it was picked up early, I am surviving and moving on with my life.” Those testimonials have been incredibly powerful in changing the public perception.
In terms of progress in access to cancer care, in Kenya we’ve been incredibly fortunate. Our national cancer control programme has done a lot of work developing guidelines around treatment, screening, specimen handling… looking at the entire continuum of care all the way from prevention through to survivorship. And our National Hospital Insurance Fund now supports some of the costs of cancer care – it’s not perfect, but it has made a difference. Over the last 10 years, we have been able to get more patients to the finishing line in terms of getting all the treatments that they require. This has gone a long way towards changing the overall perception around cancers and the long-term outcomes.
Where are we failing? We have not thought through how we invest and support the financial aspects of cancer care as much as we should. In Sub Saharan Africa we are paying three to four times more for many cancer drugs than in countries of similar income levels elsewhere, so we need to think about how we can change this. There has been some work done by different organisations, but unless we get government buy-in, these tend to be limited short-term projects. We need to work with collaborators in the region to think about how we can drop the price for our patients collectively.
We also need to think about strategies for funding cancer care; how best to invest the limited resources allocated from the National Hospital Insurance Fund? What about other sources of funding? And we need to involve other professions and sectors. We talk about prevention and about signs and symptoms for early detection, but how do we then educate the public? That’s where we need the teachers. And we need researchers to look at the variability in trends in our populations.
What should we be advocating for today? For the longest time there has been a reliance on someone else solving our problem for us. I think there is a growing recognition that we need to sit down together and figure out our problems. Yes we need collaborators to help support that, but we have to be the driver to sort out the concerns for our own populations.
This requires thinking critically about how our healthcare system can deliver the best for patients. And that should start by looking at the patient journey all the way from, ‘lady feels a breast lump’, for instance, and what are the bits and pieces that we need for her to get to hospital for a diagnosis? Do we have the pathology, the imaging? And then, how do we put her through treatment? whether its surgery, radiotherapy, chemotherapy. And then thinking through how do we progress her to survivorship, and all through that journey? What are the different aspects of care that are needed? What skillsets are required?
We also need to get governments to think about healthcare not as a cost, but an investment. Investing in early detection and timely appropriate treatment for our patients means healthier citizens living longer and being more productive, and that is a win for the economy.
This was one of eight interviews with participants of the World Oncology Forum that were conducted by Cancerworld. Click on the links below to see what the others had to say.
Advocating for accessible cancer care in the global South: are we doing this all wrong?
Nirmala Bhoo Pathy, Public health physician, University Malaya, Kuala Lumpur
“What is not being discussed is how do we improve wellbeing?”
See interview summary | See video
Felicia Marie Knaul, Co-chair of the Lancet Commission on Cancer and Health Systems, Sylvester Comprehensive Cancer Center and Director of the Institute for Advanced study of the Americas, University of Miami, Florida, President of the Mexican breast cancer advocacy group Tómatelo a Pecho
“In this post-Covid world we have the opportunity to harness technology in ways that we have never seen before”
See interview summary | See video
Srinath Reddy, Founder and Past President of the Public Health Foundation of India
“We need to make care affordable and strengthen our health workforce so we have people who can deliver the wide range of services that are needed”
See interview summary | See video
Bente Mikkelsen, WHO Director for Non-Communicable Diseases
“We should think through what is needed to ensure we have accountability, and simplify the metrics on what success looks like”
See interview summary | See video
Franco Cavalli, Founder & organiser of the World Oncology Forum, past Chair of the Scientific Committee of the European School of Oncology, past President of the UICC
“We need another approach, where governments, public spending, taxes, together with development banks play the overarching role in financing the global fight against cancer”
See interview summary | See video
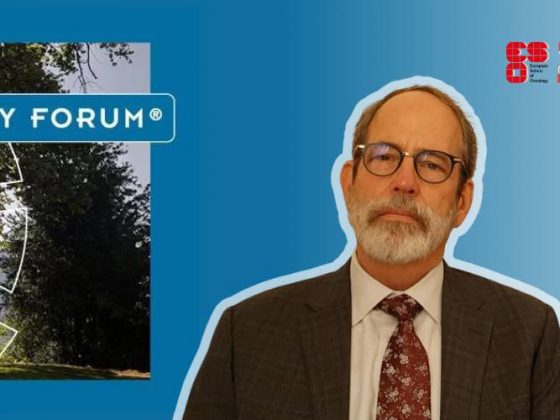
Ben Anderson, Breast Cancer Surgeon, WHO Global Breast Cancer Initiative lead
“Our role is not to tell everybody what to do; it’s to create tools so they can do this in the way that is most effective in their environment”
See interview summary | See video
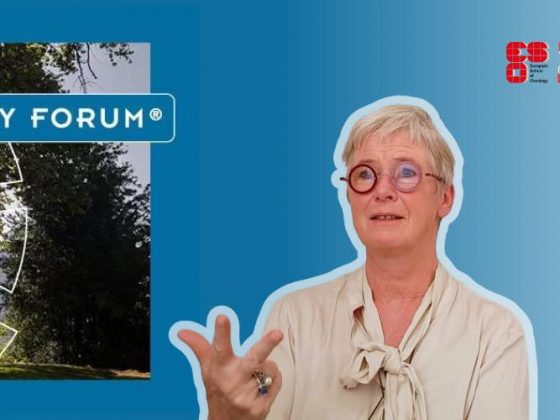
Mary Gospodarowicz, Radiation oncologist at Princess Margaret Cancer Centre, University of Toronto, co-chair of the Lancet Commission on Cancer and Health, Past President of the UICC
“We’ve been talking to decision makers for 20–30 years. It hasn’t worked. I think we now have to engage better with the public”