“Something that hit me pretty early during my residency as an oncologist was that sex in most cases is a clear-cut binary, pretty obvious biological variable affecting attitudes as well as tolerance to cancer treatment that we still rarely ‒ almost never really ‒ take into account in our everyday clinical work,” says Cecilia Radkiewicz, a medical oncologist at the Karolinska University Hospital, in Stockholm. “And yet there are so many reports suggesting that there are clinicopathological differences.”
It is now very clear that there are not only differences in the rates at which men and women are diagnosed with cancer, but also in their survival, prognosis and response to treatment. The question is what we now do about it?
Until recently, evidence of the differences in responses between men and women have been largely missing from clinical trials, particularly in drug trials, where women were generally excluded. The thalidomide disaster in the early 1960s led the US Food and Drug Administration (FDA) to issue guidelines in 1977 that essentially excluded women from all trials. But oncologists such as Radkiewicz are starting to study these sex differences ‒ in her case, using big volumes of data from multiple Swedish population-based health and demographic registers. What she and others are finding is that there are complex and multi-factoral issues involved in understanding the differences observed.
Differences in incidence and survival
With most cancer locations, men are generally diagnosed at higher rates than women. For example, 2020 OECD data for EU lung cancer rates shows the incidence is 100 per 100,000 in men, but only 45 per 100,000 in women. Some of this difference can be put down to different behaviours and comorbidities, with higher levels of smoking and drinking among men (the gender gap is smaller in Nordic countries, where behaviour differences between men and women are generally smaller).
With many cancers, men also tend to have a worse prognosis when they are diagnosed. “It’s pretty well established that men in general have a more advanced stage of diagnosis for many cancers, and cancer stage is one of the most important prognostic factors,” says Radkiewicz, who suggests men are often not as quick to seek medical advice and are more likely to ignore cancer alarm symptoms.
One cancer where women do have a poorer prognosis and more advanced stage distribution is urinary bladder cancer. “This is probably caused by a combination of patient and doctor delay, because the classic bladder cancer alarm symptom, visible blood in the urine, in a woman is not really considered an alarm symptom for a malignant disease, but in a man it is investigated much more promptly,” suggests Radkiewicz.
“Why many cancers seem more aggressive in men is a tricky question to disentangle… It’s probably not the same answer for all cancer sites”
But the stage at diagnosis is unlikely to be the whole story. A 2020 study of malignant melanoma in 1,023 patients between 1987 and 2014, for example, showed that women have better survival than men after adjusting for known prognostic factors. “There is a sex difference regarding survival in melanoma even when controlling for [diagnosis stage],” says Radkiewicz, but the reason why many cancers seem to be more aggressive in men is a tricky question to disentangle, she adds: “It’s probably not the same answer for all different cancer types.”
In bladder cancer, for example, where women have been reported to have a consistently poorer survival than men, the problem seems to be restricted to the specific subgroup of tumours that are treated with surgery in combination with chemotherapy. Radkiewicz postulates this could be linked to differences in the surgical management. “The urinary bladder looks pretty different in a woman compared to a man, because the muscle wall is substantially thinner, and this could result in faster tumour invasion of the bladder wall as well as a higher risk of complications in bladder cancer surgery in women compared to men,” she suggests.
A recent study of outcomes in gastric and oesophageal cancer surgery found differences in the treatment strategies used for men and women. In addition to significant sex differences in tumour location, female patients with oesophageal adenocarcinoma less frequently received neo-adjuvant therapy to shrink their tumours.
One explanation for differences in survival rates is the cancer-promoting effect of sex hormones. “We know that testosterone is a growth factor… and maybe it stimulates tumour aggressiveness,” says Radkiewicz. Drops in oestrogen levels after menopause may explain different incidences and survival in different age groups of women, but evidence shows this can be only part of the story, as there are differences between survival rates for boys and girls in glioblastoma, for example, which are unlikely to be attributable to sex hormones.
Physiology and hormones are not the only biological differences between men and women though. Radkiewicz refers to the findings of a retrospective study she did of lung adenocarcinoma, which she believes indicates that it is “a different disease in women [compared to men], maybe with a different risk factor profile.” Based on 23,465 records in the Swedish lung cancer register from 2002 to 2016, the study showed that the women were on average younger, and more likely to be non-smokers, in better health and more often EGFR positive, whilst men had a consistently poorer prognosis, even after adjusting for the stage of disease progression. While there was insufficient data to demonstrate that the distribution of biomarkers that drive the difference in survival are actually different between men and women patients, Radkiewicz says, “Our study supports that there are tumour biology differences.”
Glioblastoma provides further evidence for very different genetic tumour profiles in men and women, which may explain the differences in incidence and survival. Men are likely to develop more aggressive forms of glioblastoma and at a higher rate. In 2019, Joshua Rubin from Washington University School of Medicine in St. Louis, discovered that particular tumour genomic profiles were associated with increased survival, but which profiles were the most favourable differed between the sexes. In women, the best survival (3 years) was found with tumours expressing the least integrin genes (which produce receptors for cell attachment), whereas in men the best survival (18 months) was found with tumours that had low expression of cell-proliferation signalling genes.
Differences in treatment response
The differences in cancer biology are becoming clear, but there are also differences in how men and women respond to treatment, particularly in relation to the levels of toxicity experienced. This has been investigated by Anna Dorothea Wagner, a gastrointestinal cancer specialist and expert in gender medicine at the University Hospital of Lausanne, Switzerland. Gender medicine studies how diseases differ between men and women. From her clinical observations she saw a higher percentage of women than men hospitalised due to the toxicity of their cancer treatment. “Up to now, we really considered men and women as [the same], and I had the impression that this is not right,” says Wagner.
“In oncology, there is a lack of knowledge… there are a few reports about higher toxicity in women, but very few authors have investigated this topic systematically,” she says. Wagner is starting to change this. An analysis of data amalgamated from four chemotherapy trials for oesophagogastric cancer confirmed her suspicions. She found that serious nausea and vomiting (grade 3 or above) was experienced by 16.7% of female patients, but only 9.5% of male patients. All grade toxicities were also significantly higher among women than men for diarrhoea, stomatitis and alopecia, with a trend towards significance in neutropenia and febrile neutropenia. A separate study of early-stage colon cancer using a database of 28,636 patients also confirmed that women are at greater risk for the majority of toxicities.
Women appear to be more susceptible to the toxicity of different types of chemotherapy drugs, including increased risk of acute haematologic toxicity, and toxicities such as mucositis, nausea, vomiting, alopecia and cardiotoxicity. This seems to be the case among patients treated for colorectal, small-cell and non–small-cell lung cancers, Hodgkin lymphoma, glioblastoma, Ewing sarcoma and osteosarcoma. There is also evidence of differences in children, with girls treated for acute lymphoblastic leukaemia experiencing higher rates of toxicity than boys, showing this is unlikely to be just an issue of size.
“About 20% of anticancer drugs have differences in pharmacokinetics, with more rapid elimination in men, leading to higher plasma levels in women”
Wagner says sexual dimorphism in drug response is not unique to oncology drugs, and is seen across medicine, due to clear differences in how women and men metabolise drugs, and their sensitivity to them. “We know today that about 20% of anticancer drugs have differences in pharmacokinetics, with more rapid elimination in men, leading to higher plasma levels in women, and these differences are probably responsible for higher toxicities at least in in part,” explains Wagner. Both liver and renal function differ between men and women, and women have approximately 15% more body fat than men and greater plasma volume and organ blood flow.
But so far there have been few attempts to characterise these differences, including their impact on the metabolism of anticancer drugs systematically. “We can’t generally say that all toxicities are occurring at a higher grade and higher rate. I would rather describe it as a potential modulation of the toxicity profile of anticancer drugs,” says Wagner. To really understand this requires an analysis of large databases, she adds.
Currently, the formula used for calculating chemotherapy doses is identical for men and women. “We estimate something called the body surface area, that we use to calculate the dosage,” explains Radkiewicz. “We want to give men and women the same serum level of drug, so the aim is to dose [based on] the fat-free body mass, but we know that women anatomically have more body fat compared to men.” The lower female lean body mass, plus differences in liver and renal turnover in men, could mean that women are receiving higher drug plasma levels and therefore experiencing greater toxicities.
It also may explain why women seem to have a higher response to chemotherapy for some types of cancers. There is also the possibility that lower rates of toxicity in men could be a sign of underdosing, and this in itself could explain their poorer prognoses. “We’ve found in colorectal cancer that this is not the case,” says Wagner. “Despite higher toxicity and higher drug levels of fluorouracil, in colorectal cancer women do not have a higher treatment efficacy. So at the moment there are still more questions than answers.” She thinks there is certainly a need to investigate gender-specific treatment strategies more closely.
In addition to the biological differences, Wagner is also considering whether there are physician biases in the way men and women are treated that might also explain some of the differences in outcomes. “We looked at treatment allocation of men and women with curatively treatable oesophageal and gastric cancers in a population-based study and we found that, among patients with lower oesophageal adenocarcinoma, which is a disease much more frequently arising in men, the women who had this disease have a 20% lower probability of being allocated to curative treatments, such as surgery and chemoradiation. They have a less favourable prognosis because they less often get curative treatments,” says Wagner.
“The optimal timing in women differed by about six hours that in men, which likely impact on tolerability, dose intensity and efficacy”
Another curious sex difference can be found in the field of chronomedicine ‒ where drugs are administered at times that line up with patients’ circadian cycles, to improve efficacy and reduce toxicity. Oncologist Francis Lévi from the University of Warwick has been studying the topic for decades, and says recent trials have shown that the optimal drug delivery time differs between men and women. In 2012, Lévi demonstrated that administering infusions of the FOLFOX drug combination of folinic acid (leucovorin), fluorouracil (5FU) and oxaliplatin to treat metastatic colorectal cancer at a specific time of day was beneficial to men, but detrimental to women. A similar study in 2020 with the addition of the topoisomerase I inhibitor, irinotecan, to a FOLFOX regime also showed sex-based differences, with men doing better when infused in the morning and women in the afternoon. “The optimal timing in women differed by about six hours to the optimal timing in men, and this has a likely impact not only on tolerability, but also on dose intensity and efficacy,” says Lévi.
Differences in immune systems
Many cancer patients are now treated with immunotherapies, and questions about whether men and women respond differently to these therapies are also being investigated. Different responses might not be a surprise. “We know that there are immunological differences between men and women. If we extrapolate to infectious and autoimmune diseases, we know that men have a higher risk for most infectious diseases, and also poorer outcomes, while autoimmune diseases are more frequently diagnosed in women,” says Radkiewicz.
Women have a more active immune surveillance system, which could explain why their cancer incidences are lower and survival higher than men’s. A 2020 study of sexual dimorphism in colon cancer notes that there are more T cells found in samples taken from women than men, indicating a stronger immune response.
So far, evidence indicates that immune checkpoint inhibitors such as nivolumab and pembrolizumab, on their own, tend to be more effective in male cancer patients compared to female, perhaps because in women the tumour environment is initially not immunosuppressed to the same extent as in men. A meta-analysis of data by Fabio Conforti, from the European Institute of Oncology in Milan, showed that, when combined with chemotherapy, women’s survival rates improved. He suggests this is because the chemotherapy increases the mutational load of tumour cells and therefore makes the cells better targets for elimination by their more active immune systems.
These early results do show that there may need to be different strategies for treating men and woman with immunotherapies
These early results do show that there may need to be different strategies for treating men and woman with immunotherapies ‒ with therapies for men focusing on reversing immunosuppressant tumour environments, and those for women focusing on increasing the antigenicity of tumour cells. But there is clearly a long way to go before the factors involved are fully understood and the best treatment strategies developed.
Towards gender-adapted treatments
Given what we know, is it time to start treating cancer in men and women differently? “Not yet,” answers Wagner. She thinks much more work is needed first, to understand how the patient’s biological sex modifies treatment effects and the tumour biology. “When we have understood this, we have to think about how we can modify the treatment according to the patient’s sex to improve the balance between efficacy and toxicity in both men and women on the basis of what we have learned.” She also wants more investigation into patient and physician attitudes, and how unconscious biases related to gender may be impacting treatment decisions.
One area where changes might be warranted is in chemotherapy dosing. “You can estimate the individual body composition today very cheaply and relatively precisely by CT scans,” notes Wagner. “This is something you can take into account in decision making for dosing of chemotherapy drugs, but at the moment, this is not done. We need randomised clinical trials investigating sex-specific dosing strategies in oncology.”
“For more than half of the studies, the question of whether there are any potential sex differences has not been addressed at all”
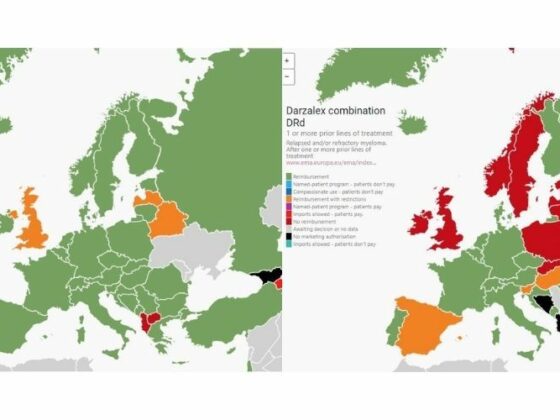
With gender being perhaps the most basic biological variable, and one that can easily be assessed with very high precision and low cost, Wagner argues there is no reason to ignore it. The 2014 European Clinical Trials Regulation was designed to improve imbalances, requiring that the subjects participating in a clinical trial should represent the population groups that are likely to use the medicine. Today many clinical trials still do not report results by sex. “We found that, for more than half of the pharmacokinetic studies, the question of whether there are any potential sex differences has not been addressed at all… this is really something I hope will be changed in the future,” says Wagner. Radkiewicz argues that, where the data is available, we should also now go back and reanalyse existing data to stratify by sex.
Understanding the genetic footprint of cancer is the aim of the burgeoning field of precision medicine. “We have made a lot of progress by exploring the molecular biology of the tumour,” says Wagner, “but the question of how the biology of the host influences the tumour, that has, unfortunately, not been studied with the same enthusiasm. So there is some work to do to catch up.”
In 2018 Wagner started this process and held an ESMO workshop, ‘Gender medicine meets oncology,’ to discuss the implications for clinical practice and research in oncology. Clearly there are multi-faceted and complicated factors involved, but after many years of neglect she hopes that the benefits and harms of anticancer treatments will now be evaluated separately for men and women. In an age of precision medicine, we can no longer assume that the effect of a given treatment is the same in men and women. “In oncology, the balance between benefits and risks is often quite subtle, and it’s really important to be sure that we have statistically significant benefits in both sexes and the risks are acceptable,” she concludes.